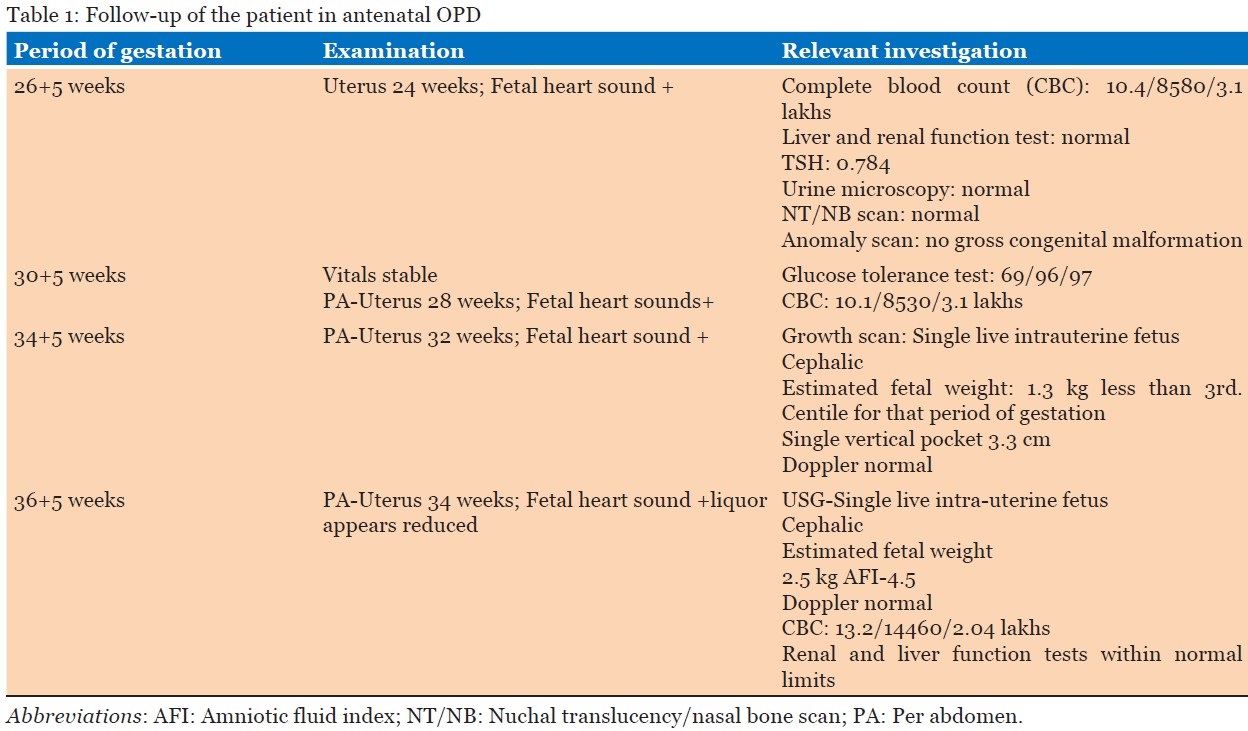
|
Case Report
A simple cost-effective method of endoscopic clearance of large blood clots in upper gastrointestinal bleeding
1 MBChB, House Officer, Health New Zealand, Palmerston North, New Zealand
2 Registered Nurse, Department of Gastroenterology, Palmerston North, New Zealand
3 MBBS, MMedSc, FRACP, Consultant Gastroenterologist, Palmerston North, New Zealand
Address correspondence to:
Shaoyi (Bessie) Zhang
MBChB, House Officer, Health New Zealand, Palmerston North,
New Zealand
Message to Corresponding Author
Article ID: 101500Z01SZ2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Zhang S, Crooks J, Khan A. A simple cost-effective method of endoscopic clearance of large blood clots in upper gastrointestinal bleeding. Int J Case Rep Images 2025;16(1):64–67.ABSTRACT
Introduction: Patients with upper gastrointestinal (GI) bleeding with large clots and associated food can make clearance and adequate visualization via the standard gastroscope very challenging. There are a few proprietary systems for large clot clearance marketed for adjunct use in endoscopy; however, world-wide availability as well as general affordability can be difficult. Advancement in simple methods to safely and effectively clear the upper GI tract for good visualization is hence important and can prevent mortality and significant morbidity in severe GI bleeding.
Case Report: An 84-year-old patient with known end-stage achalasia presented with hematemesis and worsening dysphagia. Gastroscopy under general anesthetic found large amount of food bolus and blood clot in the dilated esophagus precluding further advancement. An overtube was used to facilitate repeated scope passages. A combination of endoscopic suction, irrigation, snare use, and Roth Net use provided little improvement in clearance. Hence a nasogastric (NG) tube was inserted via the overtube into the esophagus under direct visualization. With a combination of endoscopic irrigation and direct high suction with the NG tube, the food and clot were broken down and cleared effectively.
Conclusion: Compared to traditional extraction of blood clots with associated food in piecemeal fashion, this technique of incorporating direct suctioning from the NG tube with irrigation from the gastroscope is a simple and efficient way to clear large clots and food from the upper GI tract. The equipment needed is standard equipment available in any acute endoscopy suite.
Keywords: Blood clots, Endoscopy, Food bolus, Upper GI bleeding
Introduction
Patients presenting with upper gastrointestinal (GI) bleeding and large clots in the GI tract with associated food can make clearance and adequate visualization via the standard gastroscope very challenging. Managing a food bolus obstruction with associated upper GI bleeding in a patient with motility disorder can be complicated needing effective teamwork and the use of various endoscopic accessories. Achalasia is an esophageal motility disorder leading to esophageal stasis from aperistalsis. In end stage achalasia, the esophagus can be severely dilated and desensitized, leading to significant amount of retained food in the event of food bolus obstruction. Food bolus obstruction can lead to mucosal irritation, esophagitis, and bleeding which usually requires a prolonged procedure due to efforts to get good visualization and clearance. There is currently no curative treatment to restore the native peristalsis [1], and surgical options can be high risk in certain patients. Hence patients may tend to present with food bolus obstruction requiring intervention. This can be associated with esophageal damage or inflammation and upper GI bleeding. Prolonged food impaction decreases the likelihood of successful removal and risk of serious complications including perforation [2]. There are a few proprietary systems for large clot clearance marketed for adjunct use in endoscopy; however, world-wide availability as well as general affordability can be difficult. Advancement in simple methods to safely and effectively clear the upper GI tract for good visualization is hence important and can make the difference between life and death in severe GI bleeding.
Case Report
An 84-year-old European woman with a history of end stage achalasia and surgical myotomy decades ago presented to the Emergency Department (ED) with hematemesis. She was on warfarin for chronic atrial fibrillation. Her hemoglobin level was 140 g/L. She continued to be nauseous and had lumpy discomfort sensation in lower chest and epigastric region. Due to the presenting symptoms, warfarin was reversed in the ED and intravenous omeprazole was started.
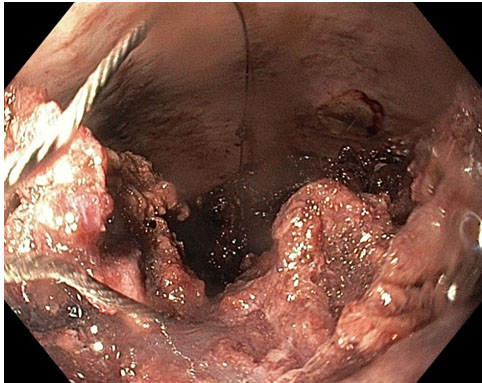
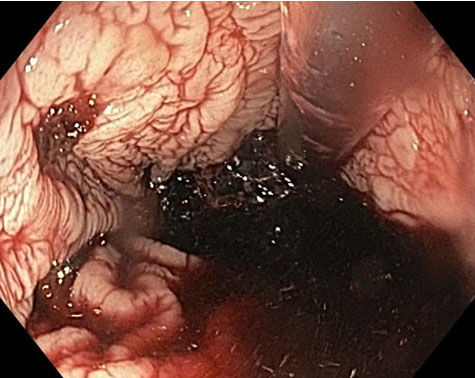
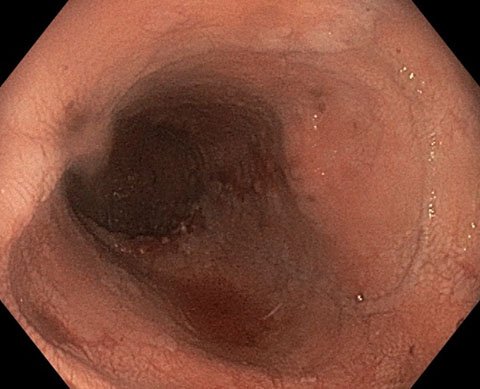
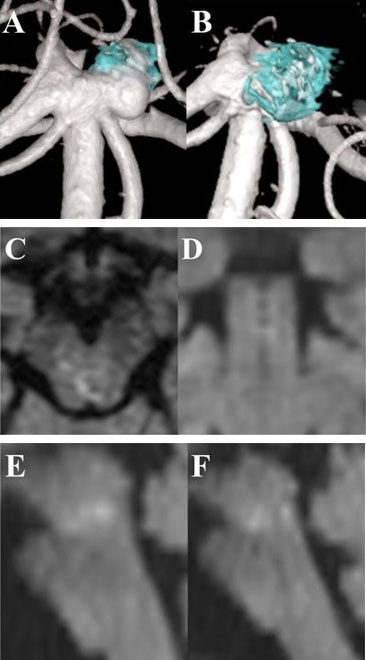
Gastroscopy was done under general anesthesia. In this procedure a gastroscope (GIF-H190; Olympus, Center Valley, PA, USA) and an esophageal overtube were used (Guardus Overtube; Steris, Mentor, OH, USA). Gastroscopy found a large amount of food bolus and blood clot in the dilated esophagus precluding further advancement of the gastroscope. The gastroscope was removed, and an overtube was fitted. The scope and overtube were then reinserted via the mouth and advanced to the esophagus to facilitate repeated passages of the scope. There was a large amount of organized clot and food in the entire esophagus. Due to this scope passage to the lower esophagus was not possible. Large clots with food were snared, suctioned, and manipulated to allow reasonable capture in repeated Roth Net passes (Figure 1). A combination of endoscopic suction, irrigation, snare use, and Roth Net use provided little improvement in clearance. Hence a nasogastric (NG) tube was inserted via the overtube into the oesophagus under direct visualization being following by the gastroscope (Figure 2). With adequate lubrication, the overtube can easily accommodate the standard gastroscope and an NG tube (Figure 3). The NG tube was connected to wall suction. The NG tube can be manipulated back and forth controlled at the site of insertion in the overtube to ensure adequate and—to some degree—targeted suction. With a combination of endoscopic irrigation and direct high suction with the NG tube, the food and clot were broken down and cleared effectively.
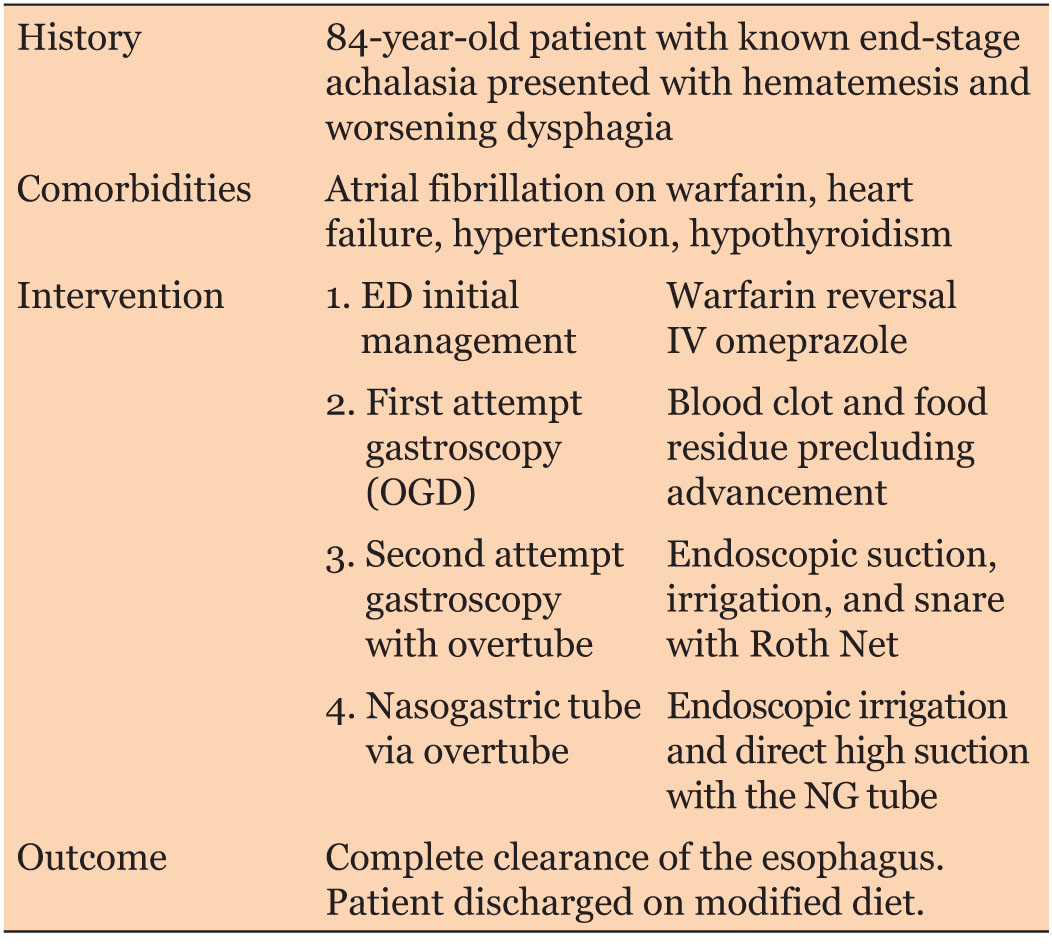
Further Roth Net passes with suction and irrigation resulted in complete clearance of the esophagus (Figure 4). One 7 mm esophageal ulcer with clean base in the lower esophagus, along with several erosions along the length of the esophagus was deemed to be the source of bleeding. The endoscope was advanced to the duodenum with no other source of bleeding found. The gastroesophageal junction was wide open after clearance. The obstruction was due to a combination of ineffective esophageal peristalsis, prolonged stasis in the esophagus of large pieces of likely ineffectively chewed food accumulating over time in a severely dilated esophagus. The patient was kept in the hospital for two more days and subsequently discharged home on a modified diet (Table 1).
Discussion
Compared to traditional extraction of blood clots with associated food in piecemeal fashion, this technique of incorporating direct suctioning from the NG tube with irrigation from the gastroscope is a simple and efficient way to clear large clots from the upper GI tract. Guideline advises against pushing a food bolus without examination of the esophagus distal to the obstruction first due to risk of perforation [2]. Extraction is traditionally done by grasping devices in piecemeal fashion, which is time consuming and even more challenging with friable soft food bolus and blood clots. Similar techniques were only reported in two other case reports: where one of them used a 32G Robinson drain tube instead of the NG tube [3] but this was only for blood clots while in our case there was a large amount of food in the dilated esophagus as well. Another case report mentions a suction tube with cut tip taped with the endoscope [4], both reported successful esophgeal clearance outcome. A small study from Japan involving 11 patients planned for peroral endoscopic myotomy applied a technique of taping a cut tip gastric tube to a super-slim gastroscope to suction out food debris under direct vision, and found it to be a safe and effective way to clear the food debris from the esophagus. However, the study did not discuss the role of irrigation in combination with suctioning and was performed on patients with less severe achalasia presenting electively for procedure instead of acute presentations [5].
Conclusion
Compared to traditional extraction of blood clots with associated food in piecemeal fashion, this technique of incorporating direct suctioning from the NG tube with irrigation from the gastroscope is a simple and efficient way to clear large clots and food from the upper GI tract. The equipment needed is standard equipment available in any acute endoscopy suite. To further validate this technique for wider application, future trials with larger sample size comparing the efficacy and safety of the novel method with the traditional piecemeal extract method would be needed.
REFERENCES
1.
DeSouza M. Surgical options for end-stage achalasia. Curr Gastroenterol Rep 2023;25(11):267–74. [CrossRef]
[Pubmed]

2.
ASGE Standards of Practice Committee; Ikenberry SO, Jue TL, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73(6):1085–91. [CrossRef]
[Pubmed]

3.
Abbott C, Botha AJ. A novel approach to oesophageal clot removal. Ann R Coll Surg Engl 2010;92(1):75–6. [CrossRef]
[Pubmed]

4.
Mahmood S, Tazinkeng N, Holzwanger EA, et al. Enhanced suction for removal of esophageal food impaction. VideoGIE 2023;8(8):298–300. [CrossRef]
[Pubmed]

5.
Tanaka S, Kawara F, Toyonaga T, et al. A novel method of endoscopic-assisted esophageal clearance in advanced achalasia. Endosc Int Open 2018;6(1):E86–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Shaoyi (Bessie) Zhang - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jackie Crooks - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Afrasyab Khan - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Shaoyi (Bessie) Zhang et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.