|
Case Report
Intramedullary arachnoid cyst: A rare cause of medullary compression
1 Resident in Neurosurgery, Department of Neurosurgery, Fann Teaching Hospital, Cheikh Anta Diop Avenue, Postal Address 5035, Dakar, Senegal
2 Associate Professor of Neurosurgery, Department of Neurosurgery, Idrissa Pouye General Hospital, Grand Yoff, Postal Address 3270, Dakar, Senegal
3 Neurosurgeon, Department of Neurosurgery , Idrissa Pouye General Hospital, Grand Yoff, Postal Address 3270, Dakar, Senegal
4 Neurologist, Department of Internal Medicine, Idrissa Pouye General Hospital, Grand Yoff, Postal Address 3270, Dakar, Senegal
Address correspondence to:
Oscar Niyonzima
MD, Resident in Neurosurgery, Department of Neurosurgery, Fann Teaching Hospital, Cheikh Anta Diop Avenue, Postal Address 5035, Dakar,
Senegal
Message to Corresponding Author
Article ID: 101323Z01ON2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Niyonzima O, Sakho MG, Fondo AI, Faye M, Nzisabira JM, Bakhoum M. Intramedullary arachnoid cyst: A rare cause of medullary compression. Int J Case Rep Images 2022;13(2):35–38.ABSTRACT
This clinical case of intramedullary arachnoid cyst is the second reported case in Senegal. It concerns a 50-yearold woman, with no particular history, admitted for back pain associated with intermittent spinal claudication. The physical examination showed a dorsal spinal syndrome, spastic paraparesis, hypoesthesis under T9 sensitive territory with bilateral Babinski sign. Cutaneous-abdominal reflexes were abolished at T8. Magnetic resonance imaging (MRI) revealed an intramedullary cyst formation. The patient was operated on the day after her admission by a posterior approach with scopic tracking. She underwent a laminectomy from T7 to T9. Thereafter the cyst has been removed, then discharged three days after the surgery. The clinical follow-up showed a full recovery.
Keywords: Arachnoid cyst, Intramedullary, Medullary compression
Introduction
Intramedullary arachnoid cyst is one of the rare causes of slow cord compression [1],[2],[3]. The topography is most often extra- or intradural. Intramedullary location is exceptional. As a benign lesion, its etiopathogenesis is not yet well understood. It is often congenital but can also be acquired (trauma or inflammation) [4]. Its symptomatology is represented by the picture of a medullary or radicular compression. The presumptive diagnosis is obtained by magnetic resonance imaging (MRI) [5]. Surgery is the treatment of choice [1].
We report a case of arachnoid cyst successfully treated in the Department of Neurosurgery at the Grand Yoff General Hospital.
Case Report
This is a 50-year-old female patient, with no previous history, admitted for back pain at T8–T9, intermittent spinal claudication with progressive reduction in walking perimeter for 15 months. The physical examination on admission showed a good general condition, a dorsal spinal syndrome, spastic paraparesis rated at 4/5, hypoesthesis under T9 sensitive territory, increased patellar and Achilles reflexes. A bilateral Babinski sign was also noted. Cutaneous abdominal reflexes were abolished at T8. There were no sensory disturbances. Anal sphincter tone was normal. The rest of the examination was unremarkable.
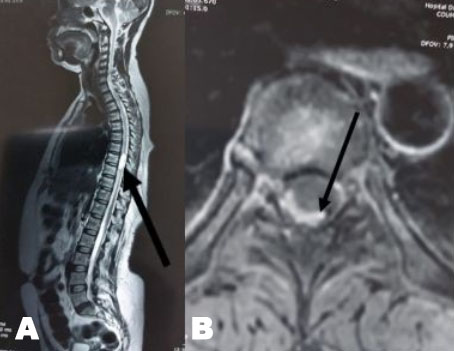
Spinal cord MRI revealed an intramedullary cystic formation at T8, measured 9.6 × 9.7 mm axially for a height of 29.3 mm. The lesion was hypointense on T1, hyperintense on T2, and unenhanced after injection of gadolinium (Figure 1A and Figure 1B).
The patient was operated on the day after her admission by a posterior approach with scoped tracking. She underwent a laminectomy from T7 to T9. After opening the dura mater opposite the posterior medial sulcus of the medulla, a large medulla appearance was noted (Figure 2).
A posterior medial myelotomy was performed to visualize a pearly white, translucent and avascular intramedullary mass (Figure 2). An aspiration of the cystic content associated with a partial excision of its shell was performed, thus allowing for spinal cord decompression. The cystic content was reminiscent of cerebrospinal fluid. The cyst had no communication with the subarachnoid spaces. Cytochemical analysis of the puncture fluid showed aspects of normal cerebrospinal fluid and the anatomopathological results confirmed the arachnoid cyst by showing the presence of arachnoid cells with no malignant cells (Figure 3).
The postoperative course was simple. The patient was discharged four days after the operation with full recovery of motor strength.
Discussion
Intramedullary arachnoid cyst is a benign but rare condition [1],[4]. Its origin is not well known. It appears to be congenital in most cases, but it can be acquired, especially in the case of trauma and inflammation such as arachnoiditis, or even idiopathic [3],[6]. In our patient, no etiology was found. The majority of intradural cysts are located in the thoracic region (80%), which is the case for our patient, the cervical region is involved in 15% of cases and the lumbar region in 5% of cases [1].
Symptoms are related to compression of the spinal cord and nerve roots, resulting in neuralgia and neurological deficits that are usually slowly progressive due to the slow and continuous increase in volume, which is consistent with the literature [3],[7],[8]. Magnetic resonance imaging is the examination of choice for any intrarachid lesion. It allows better mapping of the lesion [3],[4]. It also allows the exact topography of the lesion, its size, extent, and relationship with the spinal cord to be determined noninvasively. The imaging appearance is that of an extraor intradural lesion, intramedullary form is exceptional; it appears hyposignal in T1, hypersignal in T2, and does not enhance on gadolinium injection [2],[8],[9]. The recommended surgical technique is to evacuate the cystic contents and to remove as much of the cystic wall as possible, leaving the portion adherent to the spinal cord in place to avoid damaging the healthy spinal cord tissue, thus allowing decompression of the spinal cord [1]. This technique was also used in our patient. The evolution was marked by regression of the initial clinical signs as reported in most cases in the literature [10].
Conclusion
Intramedullary arachnoid cyst is a benign and rare lesion, but it can lead to significant neurological disorders if not managed early. Our patient has been treated early which allowed a complete recovery.
REFERENCES
1.
Goyal A, Singh AK, Singh D, Gupta V, Tatke M, Sinha S, Kumar S. Intramedullary arachnoid cyst. Case report. J Neurosurg 2002;96(1 Suppl):104–6. [CrossRef]
[Pubmed]

2.
3.
Ghannane H, Haddi M, Aniba K, Lmejjati M, Aït Benali S. Symptomatic intramedullary arachnoid cyst. Report of two cases and literature review. [Article in French]. Neurochirurgie 2007;53(2-3 Pt 1):54–7. [CrossRef]
[Pubmed]

4.
Nabors MW, Pait TG, Byrd EB, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 1988;68(3):366–77. [CrossRef]
[Pubmed]

5.
Sharma A, Sayal P, Badhe P, Pandey A, Diyora B, Ingal H. Spinal intramedullary arachnoid cyst. Indian J Pediatr 2004;71(12):e65–7.
[Pubmed]

6.
Alugolu R, Arradi V, Sahu BP. Intramedullary arachnoid cyst in an adult: Case report and review. Asian J Neurosurg 2016;11(1):70. [CrossRef]
[Pubmed]

7.
Kataria R, Sinha VD, Chopra S. Intramedullary arachnoid cyst: Report of two cases. Neurol India 2012;60(1):123–4. [CrossRef]
[Pubmed]

8.
Diyora B, Kamble H, Nayak N, Dugad P, Sharma A. Thoracic intramedullary arachnoid cyst. Neurol India 2010;58(6):964–6. [CrossRef]
[Pubmed]

9.
Panwar N, Purohit DK, Sharma S, Chopra S. Symptomatic thoracic intramedullary arachnoid cyst: “A rare entity” report of two cases with short review of literature. J Neurosci Rural Pract 2019;10(2):306–11. [CrossRef]
[Pubmed]

10.
Baeesa S, Aljameely A. Intramedullary arachnoid cyst of the cervical spine: Case report and literature review. Arq Bras Neurocir 2017;36(4):256–9. [CrossRef]

SUPPORTING INFORMATION
Author Contributions
Oscar Niyonzima - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Magatte Gaye Sakho - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Alidji Ibrahima Fondo - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohameth Faye - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jean Michel Nzisabira - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mbagnick Bakhoum - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Oscar Niyonzima et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.