|
Case Report
Epidermoid cyst arising in the mandibular ramus: A case report
1 Department of Dentistry and Oral Surgery, Federation of National Public Service Personnel Mutual Aid Associations, Tachikawa Hospital, Tokyo, Japan
2 Department of Dentistry and Oral Surgery, Keio University School of Medicine, Tokyo, Japan
Address correspondence to:
Seiji Asoda
DDS, PhD, Department of Dentistry and Oral Surgery, Keio University School of Medicine, 35 Shinanomachi, Shinjyuku-ku, Tokyo 160-0016,
Japan
Message to Corresponding Author
Article ID: 101271Z01FH2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Homma F, Karube T, Usuda S, Endo T, Asoda S, Kizu H. Epidermoid cyst arising in the mandibular ramus: A case report. Int J Case Rep Images 2021;12:101271Z01FH2021.ABSTRACT
Introduction: Dermoid and epidermoid cysts are developmental lesions derived from the ectoderm. In acquired elements, trauma and inflammation are hypothesized mechanisms of onset. In the oral region, these cysts mainly develop in the soft tissues such as floor of the mouth, moreover, it is relatively rare in the mandible. Among them, it is extremely rare in the ramus.
Case Report: A 48-year-old woman visited dental clinic because of occlusal pain of the left wisdom tooth. The panoramic X-ray film showed an oval-shaped radiolucent area in the left mandibular ramus. Computed tomography revealed radiolucent area in the left mandibular ramus, moreover, there was no bone destruction. Magnetic resonance imaging revealed a lesion measuring 18×17×21 mm in size with mixed moderate and high signal intensity on fat-suppressed T2-weighted imaging in the left mandibular ramus. Gadolinium contrast-enhanced T1-weighted imaging showed no clear enhancement. On the basis of imaging findings, cystic lesion was diagnosed. We performed cystectomy and extraction of the lower wisdom teeth under general anesthesia. Histopathologic examination of the resected specimen revealed the unilocular cyst lined keratinized squamous epithelium. There were no adnexal skin structures such as sweat grand, sebaceous glands, and hair follicles. In addition, the lesions were not associated with teeth and were found only in the mandibular ramus. From these results, it was finally diagnosed as the epidermoid cyst. Three years and six months have passed, but there is no recurrence and a radiolucent area in the panoramic X-ray film shows increased radiopaque. Computed tomography revealed that the defect of the bone is reduced. The postoperative course was uneventful.
Conclusion: There is a large amount of literature on jaw diseases; however, we may still come across unique and unclear cases. Clinical examinations, conventional radiography, and surgical experience are not sufficient for the diagnosis of all pathologies. Our case is very rare and is a unique case in the relevant literature because the lesion was limited to the mandibular ramus above the mandibular foramen and was not associated with teeth.
Keywords: Epidermoid cyst, Mandibular ramus
Introduction
Dermoid and epidermoid cysts are developmental lesions derived from the ectoderm. Trauma and inflammation are hypothesized mechanisms involved in the onset in acquired cases. In the oral region, these cysts mainly develop in the soft tissues, such as at the floor of the mouth, and it is relatively rare to see development in the mandible and extremely rare to see it in the ramus [1]. We herein report a case of epidermoid cyst arising in the mandibular ramus.
Case Report
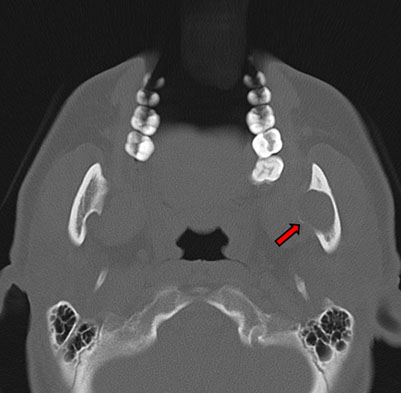
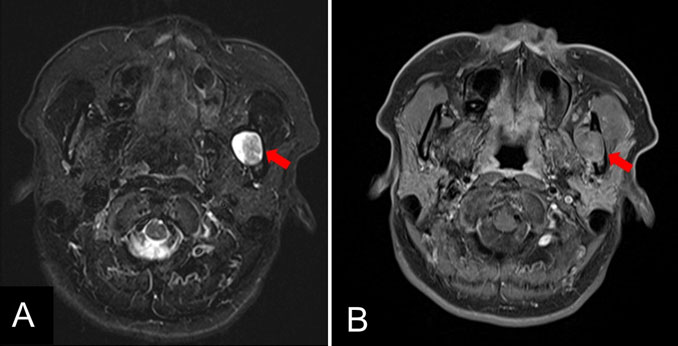
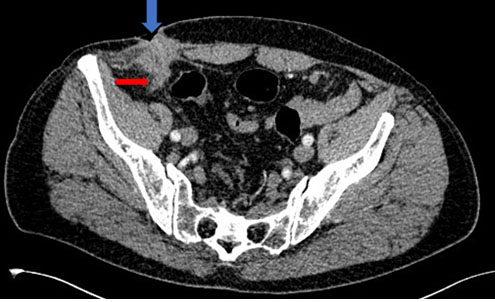
In August 2017, a 48-year-old Japanese woman visited the dental clinic because of occlusal pain in her left wisdom tooth. A panoramic X-ray showed an oval-shaped radiolucent area in the left mandibular ramus. She presented to our department for careful examination. Regarding the extraoral findings, no mass was palpable in the left mandible, and there was no dysesthesia in the left mental nerve area. Intraorally, no swelling or induration was observed inside the mandibular ramus, moreover, there was no difference between the two sides and the mucosa was a normal color. Her medical history included hyperlipidemia, iron-deficiency anemia, and diabetes. A panoramic X-ray revealed an almost circular and well-defined translucent image in the left mandibular ramus (Figure 1). Computed tomography (CT) revealed bone depression in the left mandibular ramus, and more thinning bone was seen inside. There was no obvious abnormal bone destruction. The internal density was similar to that of adipose tissue (Figure 2). Magnetic resonance imaging (MRI) revealed a lesion measuring 18×17×21 mm in size with mixed moderate and high signal intensity on fat-suppressed T2-weighted imaging in the left mandibular ramus. Gadolinium contrast-enhanced T1-weighted imaging showed no clear enhancement. Based on the clinical and imaging findings, it was likely to be a cystic lesion (Figure 3). Considering the anatomical site (it was located inside the mandibular ramus), we decided not to perform biopsy.
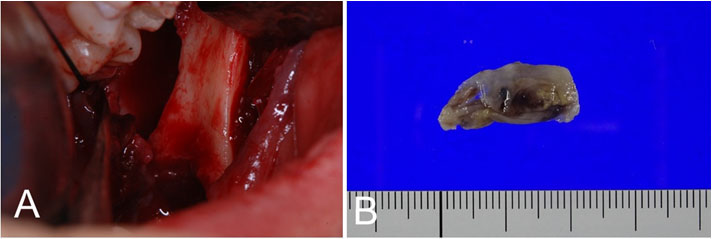
In September 2017, the patient underwent enucleation of the cystic lesion and extraction of bilateral mandibular wisdom teeth under general anesthesia. A vertical incision was made in the buccal gingiva of the left second molar, and the incision in the distal gingiva was extended to the base of the coronoid process to dissect the mucoperiosteal flap. Subsequently, the mandibular ramus and coronoid process were fully exposed. To access inside the mandibular ramus, dissection was extended to the retromandibular region so as not to destroy the thinning bone. It was relatively easy to separate the lesion from the mandible, and the lesion was removed as a single mass. The fluid in the lesion had a brownish and muddy appearance (Figure 4). In the perioperative period, the patient stopped taking hypoglycemic medication from the day before surgery, and insulin therapy, which was administered utilizing a sliding scale, was applied during the period that the patient was unable to eat. The patient started eating on the first postoperative day, and oral hypoglycemic medication was restarted on the second postoperative day with increased food intake. The blood sugar level was well controlled during hospitalization, and she was discharged on the seventh postoperative day.
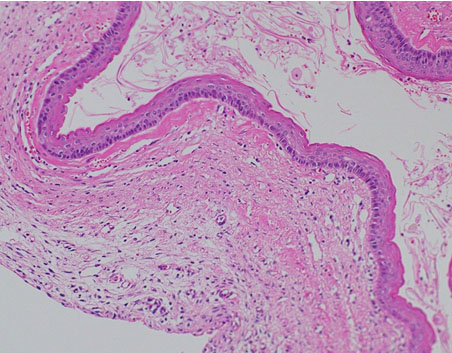
Histopathologically, the unilocular cyst was covered with thin and orthokeratinizing stratified squamous epithelium. Some parts showed mild erosion with neutrophilic infiltration in the epithelium. The cyst cavity was filled with a large amount of keratotic material, and hemorrhage, hyalinization, and mild infiltration of acute and chronic inflammatory cells were observed in the subepithelial stroma. Given the above findings, the final diagnosis was epidermal cyst.
At present, three years and six months have passed since the operation, panoramic X-ray and CT showed increased radiopacity and bone regrowth, and the postoperative course has been uneventful without recurrence (Figure 5 and Figure 6).
Discussion
Epidermoid and dermoid cysts originate from the inclusion of congenital ectodermal tissue during fetal life, or from the straying of epithelial tissue due to trauma or inflammation. The ovary and anus are the most common sites; however, these cysts may occur in various parts of the body, including the head and neck. According to Meyer's report [2], these cysts are histopathologically classified into three groups: dermoid cysts, which contain skin appendages, such as sebaceous glands, sweat glands, and hair follicles in the connective tissue, epidermoid cysts, which do not contain skin appendages, and teratoma-like cysts, which contain skin appendages, connective tissue, and respiratory and digestive tissue. There is little sex difference and most patients are around 20 years of age. Epidermoid and dermoid cysts are rare, with 7% occurring in the head and neck, 1.6% of which occur in the oral cavity [3]. The incidence in the orbits is overwhelmingly high (47%), followed by the floor of mouth (23%) and the submandibular to upper cervical region (9–24%); however, the jaw bone is considered a very rare location [4].
To the best of our knowledge, 9 cases of epidermoid cysts in the mandible have been reported in the English literature, including the present case [4],[5],[6],[7],[8],[9],[10]. Among 9 cases, 4 cases were located in the mandibular body alone, 3 cases were located in the mandibular ramus alone, including our present case, and 2 cases were located from the mandibular body to the ramus. Among these cases, ours was the only case in which the lesion was only found in the mandibular ramus, above the mandibular foramen, and was not associated with the teeth. In general, most cysts in the body of the mandible contain impacted teeth or have a history of trauma or surgery, suggesting the possibility of odontogenic factors or acquired epithelial migration. Although pericoronitis was present in this case, there was complete separation between the lesion and wisdom tooth. In addition, there have been reports of cysts that developed in the body of the mandible due to inflammation or trauma, or that were thought to have developed due to congenital migration of the ectoderm. However, the anatomical morphology and position of the inner mandibular ramus precludes the possibility of isolated development due to inflammation or trauma. Moreover, the age of the patient and the fact that there was a single layer of bone coverage suggest that the ectoderm was unlikely to have been acquired. In general, the mandible differs from other long bones in that it develops through a combination of endochondral and intramembranous ossification [11]. Considering the lack of acquired factors and the relatively rare site and asymptomatic presentation in our case, we cannot completely exclude the possibility that the malformation was caused by congenital slow development. The pathogenesis of this disease is still unclear, and further basic research is needed to clarify the mechanism.
Regarding the imaging findings, epidermoid cysts in the jawbone generally appear as a unilocular radiolucent image with well-defined borders on panoramic X-ray and CT. Magnetic resonance imaging shows a low signal intensity on T1-weighted imaging and moderate to high signal intensity on T2-weighted imaging in many cases. Since epidermoid cysts in the jawbone are relatively rare, it is difficult to differentiate them from dentigerous cysts, odontogenic keratocysts (OKC), orthokeratinizing odontogenic cysts (OOC), and ameloblastoma (unicystic type) [12],[13],[14],[15],[16]. In particular, it is difficult to histologically differentiate OKC and OOC from epidermoid cysts arising in the jawbone. However, it has been reported that OKC is histopathologically characterized by complex parakeratinization or hyperkeratosis of the lining epithelium, while epidermoid cysts are differentiated by the presence of orthokeratinization of the lining epithelium. In addition, OKC is characterized by basal cell palisading, which has been reported to be one of the features that can be used in its diagnosis [17]. In this study, OKC was excluded because the epithelial lining showed orthokeratinization. The basal cell palisading was not clear. On the other hand, it has been reported that it is difficult to differentiate between the presence of OOC and epidermoid cysts, which were newly described in the 2017 WHO classification of odontogenic tumors. In the same report, it was concluded that as long as there are reports of dermoid cysts occurring in the jawbone, the possibility of epidermoid cysts occurring in the jawbone cannot be denied, suggesting that it is difficult to differentiate between OOC and epidermoid cysts. The diagnosis of epidermoid cyst is made based on the fact that most OOCs are associated with unerupted or embedded teeth [18]; the cyst was isolated and located above the mandibular ramus in our case. Because the histopathological differentiation has not yet been fully established, it is necessary to accumulate case reports and conduct further studies.
The most common treatment for epidermoid cysts of the jawbone is surgery, and surgical removal was performed in all reported cases. Craig et al. [19] reported a method of first-stage marsupialization followed by second-stage enucleation. In our own case, enucleation was performed under general anesthesia, and the clinical course was good at three years and six months after surgery. Since recurrent cases have been reported, continuous follow-up is necessary.
Conclusion
There is a large amount of literature on jaw diseases; however, we may still come across unique and unclear cases. Clinical examinations, conventional radiography, and surgical experience are not sufficient for the diagnosis of all pathologies. Our case is very rare and is a unique case in the relevant literature because the lesion was limited to the mandibular ramus above the mandibular foramen and was not associated with teeth.
REFERENCES
2.
Meyer I. Dermoid cysts (dermoids) of the floor of the mouth. Oral Surg Oral Med Oral Pathol 1955;8(11):1149–64. [CrossRef]
[Pubmed]

3.
Janarthanam J, Mahadevan S. Epidermoid cyst of submandibular region. J Oral Maxillofac Pathol 2012;16(3):435–7. [CrossRef]
[Pubmed]

4.
5.
Takigawa T, Onuma M, Kodama M, Tanaka H. Case report of epidermoid cysts developed in the anterior and ramus regions of mandible. J Nihon Univ Sch Dent 1967;9(4):180–7. [CrossRef]
[Pubmed]

6.
Noffke CE. Implantation-type epidermoid cyst of the mandible. Dentomaxillofac Radiol 1999;28(6):383–5. [CrossRef]
[Pubmed]

7.
Jayade BV, Upadya VH, Gopalkrishnan K, Shirganvi MS. Epidermal inclusion cyst of the mandible after extraction of a third molar: Case report. Br J Oral Maxillofac Surg 2012;50(5):e72–4. [CrossRef]
[Pubmed]

8.
Toptas O, Akkas I, Tek M, Ozan F, Boran C. Intraosseous epidermoid cyst associated with impacted mandibular wisdom teeth: An uncommon entity. J Clin Diagn Res 2014;8(7):ZD31–2. [CrossRef]
[Pubmed]

9.
Loxha MP, Salihu S, Kryeziu K, et al. Epidermoid cyst of mandible ramus: Case report. Med Arch 2016;70(3):238–40. [CrossRef]
[Pubmed]

10.
Thomas M, Tremain R, Laugharne D. Epidermal cyst of the mandible: A case report. Oral Surgery 2017;10(3):171–3. [CrossRef]

11.
Beresford WA. Schemes of zonation in the mandibular condyle. Am J Orthod 1975;68(2):189–95. [CrossRef]
[Pubmed]

12.
Viswanatha B, Nayak LK, Karthik S. Cholesteatoma of the maxillary sinus. Ear Nose Throat J 2007;86(6):351–3.
[Pubmed]

13.
Chambers AA, Lukin RR, Tomsick TA. Cranial epidermoid tumors: Diagnosis by computed tomography. Neurosurgery 1977;1(3):276–80. [CrossRef]
[Pubmed]

14.
Olson JJ, Beck DW, Crawford SC, Menezes AH. Comparative evaluation of intracranial epidermoid tumors with computed tomography and magnetic resonance imaging. Neurosurgery 1987;21(3):357–60.
[Pubmed]

15.
Gualdi GF, Di Biasi C, Trasimeni G, Pingi A, Vignati A, Maira G. Unusual MR and CT appearance of an epidermoid tumor. AJNR Am J Neuroradiol 1991;12(4):771–2.
[Pubmed]

16.
Tampieri D, Melanson D, Ethier R. MR imaging of epidermoid cysts. AJNR Am J Neuroradiol 1989;10(2):351–6.
[Pubmed]

17.
Takeda Y, Oikawa Y, Satoh M, Nakamura SI. Latent form of multiple dermoid cysts in the jaw bone. Pathol Int 2003;53(11):786–9. [CrossRef]
[Pubmed]

18.
Dong Q, Pan S, Sun LS, Li TJ. Orthokeratinized odontogenic cyst: A clinicopathologic study of 61 cases. Arch Pathol Lab Med 2010;134(2):271–5. [CrossRef]
[Pubmed]

19.
Craig GT, Holland CS, Hindle MO. Dermoid cyst of the mandible. Br J Oral Surg 1980;18(3):230–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Fuka Homma - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Takeshi Karube - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shin Usuda - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tomoki Endo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Seiji Asoda - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hideki Kizu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Fuka Homma et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.