|
Case Series
Ultrasound-guided aspiration of intracranial abscess in a tertiary health institution in South-eastern Nigeria: Facing the many challenges of a resource-poor setting
1 Lecturer, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Anambra State, Nigeria
2 Professor, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Anambra State, Nigeria
3 Senior Lecturer, Department of Radiology, Nnamdi Azikiwe University, Nnewi Campus, Anambra State, Nigeria
4 Post-part 2 Fellow, Department of Radiology, Nnamdi Azikiwe University, Nnewi Campus, Anambra State, Nigeria
5 Senior Registrar, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Anambra State, Nigeria
Address correspondence to:
Sunday PU Nkwerem
Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Anambra State,
Nigeria
Message to Corresponding Author
Article ID: 101270Z01SN2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Nkwerem SPU, Emejulu JKC, Umeh EO, Umeokafor CC, Ekweogwu OC, Nwosu RC. Ultrasound-guided aspiration of intracranial abscess in a tertiary health institution in South-eastern Nigeria: Facing the many challenges of a resource-poor setting. Int J Case Rep Images 2021;12:101270Z01SN2021.ABSTRACT
Introduction: Intracranial abscesses are usually life-threatening. Minimally invasive procedures are effective especially if deep seated, located in dominant or eloquent cortex. Image guidance especially, ultrasound guidance, could suffice in resource poor setting. Absence of appropriate probes, dedicated theatre ultrasonographic setup, and technical know-how may be a drawback. We present our experience with four cases managed recently in our institution. Highlighting our limitation and efforts made to overcome this.
Case Series: Four consecutives cases, a 2-month-old baby, a 15-year-old female, a 67-year-old man, and a 2-month-old baby with a right deep frontoparietal, occipital, right fronto-parieto-occipital, and frontoparietal intracranial abscesses respectively, had ultrasound-guided aspiration of lesion using adapted transducer, together with good collaboration with the radiology department of the hospital. Procedure was successful.
Conclusion: Ultrasound guidance in resource poor setting remains a good option with due inter-disciplinary collaboration.
Keywords: Intracranial abscesses, Ultrasound guidance
Introduction
Cranial abscesses are life-threatening conditions. Mortality rate as high as 20% has been reported in some climes [1]. Increasing availability of good imaging tools, potent antibiotics, and increasing surgical intervention, appear to have improved the outcome [2]. Some of surgeries done for intracranial abscesses include craniotomy, craniectomy, ventriculostomy, burr-hole drainage, and image-guided aspiration of intracranial abscess [3]. Craniotomy and craniectomy help in easy evacuation of subdural empyema and paracranial (extradural and subperiosteal) abscesses especially if there is associated osteomyelitis [3]. Unfortunately, abscess in deep locations, dominant hemisphere, or eloquent area of the brain continue to pose challenges on the best surgical treatment. Besides, patients are occasionally too frail to undergo craniotomy and craniectomy [4]. Less invasive or more limited procedures have been shown to be efficacious [5],[6],[7].
Intraoperative image guidance reduces the need for extensive and mutilating procedure [7],[8],[9]. Neuronavigation and stereotaxy can be used intraoperatively to accurately localize intracranial abscess [8]. The problem of brain shift following durotomy may make the surgeon miss the lesion especially if it is not a big lesion. Stereotaxy and neuronavigation also require big capital base for a set up. This makes it not a readily available option in developing climes. Intraoperative computed tomography (CT) and magnetic resonance imaging (MRI) are very useful but not readily available in third world countries. Ultrasound provides a real time intraoperative image [10],[11],[12]. The technology is cheap, though may be observer dependent. Using an appropriate transducer via the fontanelles or a bone window created, the abscess could be localized and drained. The extent of aspiration could also be monitored while the procedure lasts.
We present our experience with four cases of intracranial abscess managed recently in a resource poor setting, highlighting some of the modifications done in the absence of the optimum.
Case Series
Case 1
A 4-month-old female presented with recurrent high grade fevers for one month. There was associated projectile vomiting and left-sided partial seizure as well as progressive enlargement of the head. Other aspects of the history were unremarkable. She was febrile at presentation, occipito-frontal circumference was 47 cm (normal for age was 42±2 cm). Anterior fontanelle was bulging and measured 6 cm by 6 cm.
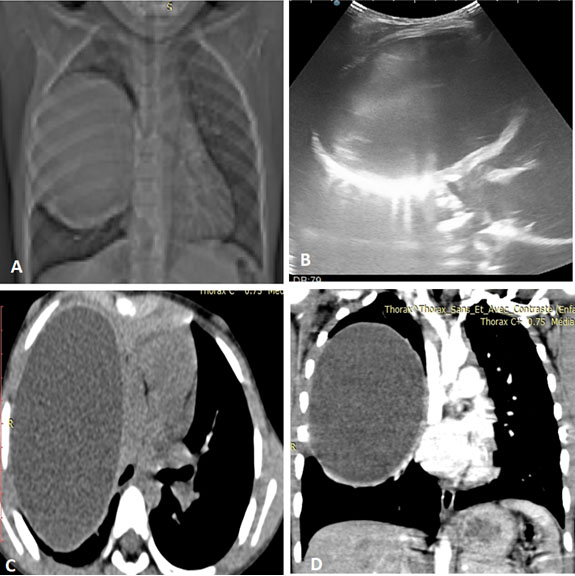
Contrast cranial CT scan done showed right deep frontoparietal cerebral abscess aborting on the falx cerebri and extending across the midline, associated with effacement of ipsilateral lateral ventricles and midline shift (see Figure 1). The abscess cavity was approached via the shortest trajectory while avoiding eloquent areas identified anatomically.
She subsequently had intravenous (IV) antibiotics, seizure prophylaxis. Operatively, she had slight extension of the anterior fontanelle to the right by bone excision (craniectomy) and ultrasound-guided drainage of right frontoparietal abscess (see Figure 2) using, a size 16 cannula and syringe. A curvilinear ultrasound probe (3.5–5 MHz) was used while an acoustic window was provided with a glove into which about 15 mL of normal saline had been poured and tied. This bag of saline was placed on the surgical wound (anterior fontanelle and craniectomy). About 70 mL of pus was aspirated. Her clinical condition improved. After about four weeks she developed hydrocephalus for which she had a shunting procedure after adequate work up.
Case 2
A 15-year-old right-handed female who presented to children emergency room with high grade fever, generalized tonic-clonic seizure, and altered consciousness of 24 hours. She had background chronic ear discharge.
At presentation, acutely ill looking, febrile (39.8C), Glasgow coma score was 12/15 (E4,V3,M6), both pupils were 3 mm and briskly reactive to light. She had right infra nuclear facio-paresis. There was also purulent right ear discharge.
Contrast cranial CT scan showed multiple intracranial ring enhancing lesion bifrontal, right parietal, and occipital sub-dural, right parafalcine ring enhanced hypodense lesion with slight brain midline shift to the left. The patient was commenced on IV antibiotics and antiseizure medication.
She subsequently had right fronto-parieto-temporal craniotomy and ultrasound-guided right occipital abscess aspiration (see Figure 3 and Figure 4). The eloquent areas of the brain were avoided.
Case 3
A 67-year-old right-handed male trader who presented with recurrent generalized tonic-clonic seizure of three weeks with associated fever. Glasgow coma score was 15/15. Cranial CT scan showed right fronto-parieto-temporal intracerebral abscess. He had right frontal mini craniectomy plus ultrasound scan-guided aspiration of frontal intraparenchymal cyst. Post-op and follow-up have been uneventful.
Case 4
A 2-month-old adopted child presented to the pediatrician with a history fever of two weeks duration. There was no seizure. Examination revealed normal occipitofrontal circumference, but bulging anterior fontanelle. Cranial CT done showed frontal and parietal ring enhancing intraparenchymal lesions. He had IV antibiotics. Parents initially declined surgery. However, after a total of two weeks of antibiotics by the pediatrician, consent for surgery was given. A repeat pre-op cranial image could not be done immediately because of financial difficulty. However, an on table transfontanelle ultrasound revealed that the cystic component had resolved. Surgery was consequently aborted.
Discussion
Worldwide, intracranial abscess still poses a significant health problem especially in developing countries [1],[5],[13], with mortality still ranging from 10% to 20% [14],[15],[16]. Frontal lobe appears to be the most common location of intraparenchymal abscess [16].
Multidisciplinary team approach, including medical and neurosurgical modalities may be needed for effective treatment. Craniotomy and craniectomy are effective surgical approaches for intracranial abscesses since they reduce the risk of reaccumulation and second surgery [4],[17],[18]. It is however associated with more morbidity [16]. Less invasive procedures like burr hole and stereotaxy have been showed to be effective [14],[16],[19].
Abscesses that are intraparenchymal and deep seated, located in dominant hemisphere or eloquent areas of the brain require precision if post-op morbidity is to be reduced. Stereotaxy is useful in abscesses that are deep seated in the thalamus, basal ganglia and brainstem, and abscesses located in eloquent regions [20]. It provides rapid access through a predetermined coordinate. It avoids the leucotomy effect that can occurs with free hand [20]. This is however not readily available in our clime. The cost and the manpower needed to sustain its use is almost not available in many developing countries. This is same for neuronavigation.
Intraoperative CT has improved the management of intracranial abscess. Intraoperative CT guidance helps in accurate localization of lesion with minimal injury to the surrounding tissues [21]. In cranial CT scan, intracranial abscess is seen as a hypodense parenchymal collection with a relatively smooth inner and outer rim which shows homogeneous peripheral enhancement on post-contrast images with associated peripheral edema. It also gives more bony details in cases of associated osteomyelitis. Its drawback is that it makes use of ionizing radiation. Intraoperative MRI scan helps to detect earlier stages of abscess formation (early and late cerebritis) during which a capsule might not be visualized. Characteristically on MRI, brain abscess appears as brain lesion which is hypointense on T1 and hyperintense on T2-weighted images with a surrounding ring enhancement that shows restricted diffusion on diffusion weighted images (DWI). Thus differentiating it from other cystic cranial lesions like cystic cranial metastasis, tumor necrosis that do not show restricted diffusion. Sequential intraoperative cranial CT or MRI scans show the progress of the reduction in the size of the intracranial abscess as the procedure is being done. Both intraoperative CT scan and MRI are not available in our setting. Occasionally, brain shift may also be a problem in sequential intraoperative image scan. In intraoperative ultrasonography, an intracranial abscess appears as a rounded hypoechoic collection with low level echoes located within the brain parenchyma which is surrounded by irregular hypoechoic areas within the white matter due to perilesional edema. Ultrasound is cheaper, readily available, hence, useful in our resource poor setting. It does not make use of ionizing radiation. However, it is operator dependent. It should be considered as a treatment modality in our environment, especially, when an acoustic window such as bony defect, burr hole, or craniotomy defect is available.
With appropriate ultrasound probes, ultrasound-guided aspiration of intracranial abscess has been done by various authors with success [22],[23],[24]. The lack of appropriate probe in a resource poor setting may be a major limitation for the procedure.
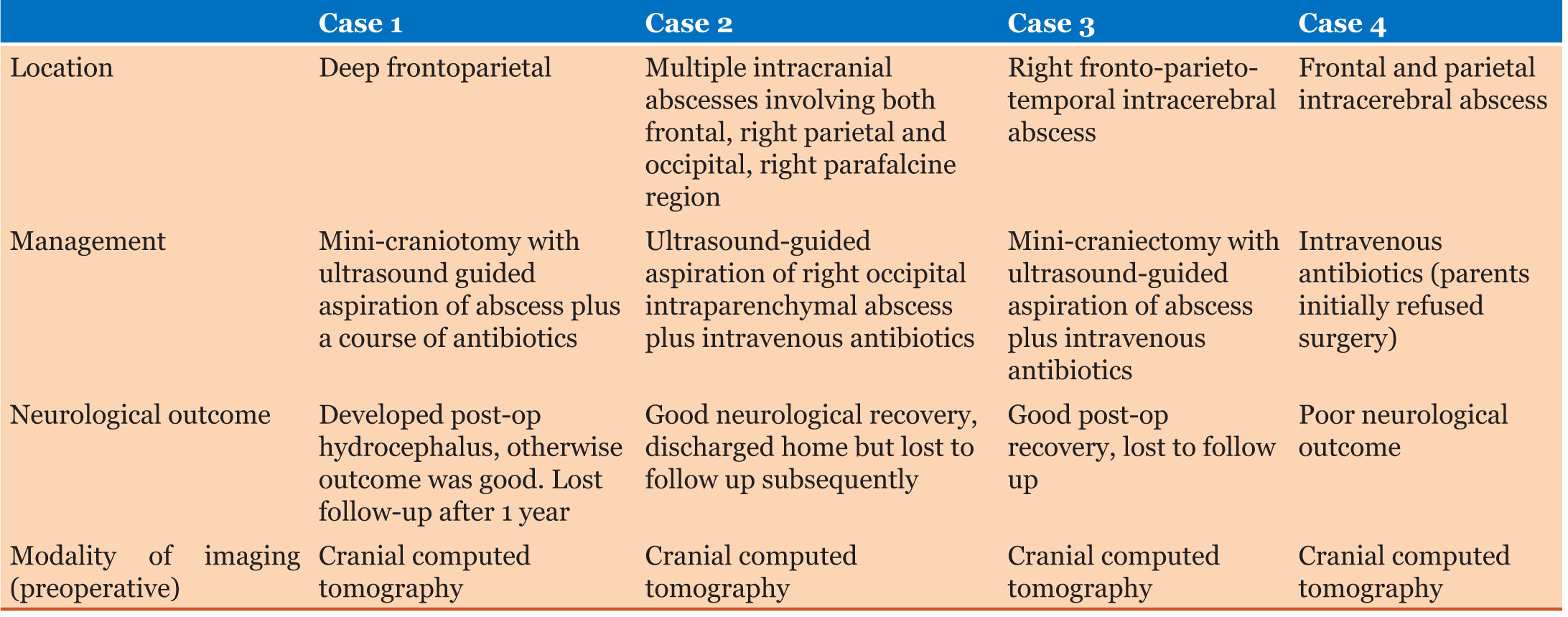
In the management of the above four cases (see Table 1 for summary), some of challenges faced included: absence of a dedicated theatre ultrasound machine, lack of appropriate transducer [small, high frequency, linear, or footprint transducer (7.5–10.0 MHz)] for the procedure, lack of expertise on the use of ultrasound machine by the operating surgeons.
The first and last challenges were overcome by adequate collaboration with the Radiology Department of the hospital. The surgery was fixed at a time when there was least traffic of patients in the Radiology Department of the hospital. Some of the cases were taken when the collaborating radiologists were off scheduled duty in the department. Second, in the absence of the appropriate small, high frequency, linear or footprint transducer (7.5–10.0 MHz), a curvilinear transducer (3.5–5 MHz) was used. The intervening bag of saline was used to improve visualization. The outcome was noted to be favorable in three cases of the cases highlighted above, before they were lost to follow-up.
Recommendations
First, there is a need for a dedicated theatre ultrasound machine. This will reduce the time interval between admission and operation. It will also reduce the risk of nosocomial infection associated with moving machine from the Radiology Department to the theatre.
Second, neurosurgeons should be encouraged to update their skills on the use of intraoperative ultrasound. This will reduce the burden on the Radiology Department.
Third, the need for the acquisition of appropriate transducer [small, high frequency, linear or footprint transducer (7.5–10.0 MHz)] for clear images cannot be overemphasized.
Conclusion
Intracranial abscesses especially deep seated abscesses can be managed by ultrasound-guided operation in our resource poor setting. There is the need, however, for capacity building to enhance surgical intervention.
REFERENCES
1.
Donaldson G, Webster D, Crandon IW. Brain abscess at the University Hospital of the West Indies. West Indian Med J 2000;49(3):212–5.
[Pubmed]

2.
Laulajainen-Hongisto A, Lempinen L, Färkkilä E, et al. Intracranial abscesses over the last four decades; changes in aetiology, diagnostics, treatment and outcome. Infect Dis (Lond) 2016;48(4):310–6. [CrossRef]
[Pubmed]

3.
Udoh DO, Ibadin E, Udoh MO. Intracranial abscesses: Retrospective analysis of 32 patients and review of literature. Asian J Neurosurg 2016;11(4):384–91. [CrossRef]
[Pubmed]

4.
Bonfield CM, Sharma J, Dobson S. Peadiatric intracranial abscesses. J Infect 2015;71(1)S42–46. [CrossRef]
[Pubmed]

5.
Levy RM. Brain abscess and subdural empyema. Curr Opin Neurol 1994;7(3):223–8.
[Pubmed]

6.
Winkler D, Strauss G, Hesse S, et al. Preoperative imaging as the basis for image-guided neurosurgery. [Article in German]. Radiologe 2004;44(7):723–34. [CrossRef]
[Pubmed]

7.
Boviatsis EJ, Kouyialis AT, Stranjalis G, Korfias S, Sakas DE. CT-guided stereotatic aspiration of brain abscess. Neurosurg Rev 2003;26(3):206–9. [CrossRef]
[Pubmed]

8.
Sharma BS, Gupta SK, Khosla VK. Current concepts in the management of pyogenic brain abscess. Neurol India 2000;48(2):105–11.
[Pubmed]

9.
Barlas O, Sencer A, Erkan K, Eraksoy H, Sencer S, Bayindir C. Stereotactic surgery in the management of brain abscess. Surg Neurol 1999;52(4):404–11. [CrossRef]
[Pubmed]

10.
Nkwerem S, Goto T, Ogiwara T, Yamamoto Y, Hongo K, Ohaegbulam S. Ultrasound-assisted neuronavigation-guided removal of a live worm in cerebral sparganosis. World Neurosurg 2017;102:696.e13–696.e16. [CrossRef]
[Pubmed]

11.
Sahoo RK, Mohanty S, Sarangi GS, Pripathy T. Percutaneous ultrasound-guided aspiration of brain abscess in an elderly male patient. Saudi J Health Sci 2016;5(1):56–9. [CrossRef]

12.
Meng XH, Feng SY, Chen XL, et al. Minimally invasive image-guided keyhole aspiration of cerebral abscesses. Int J Clin Exp Med 2015;8(1):155–63.
[Pubmed]

13.
Lu CH, Chang WN, Lin YC, et al. Bacterial brain abscess: Microbiological features, epidemiological trends and therapeutic outcomes. QJM 2002;95(8):501–9. [CrossRef]
[Pubmed]

14.
Emejulu JKC, Shokunbi MT, Malomo AO. Intracerebral abscesses: Outcome following management in the CT era. West Afr J Med 2004;23(1):54–7. [CrossRef]
[Pubmed]

15.
Sharma R, Mohandas K, Cooke RPD. Intracranial abscesses: Changes in epidemiology and management over five decades in Merseyside. Infection 2009;37(1):39–43. [CrossRef]
[Pubmed]

16.
Ndubuisi CA, Ohaegbulam SC, Mezue WC, Chikani MC, Nkwerem SP, Ozor II. Management of brain abscess: Changing trend and experience in Enugu, Nigeria. Niger J Surg 2017;23(2):106–10. [CrossRef]
[Pubmed]

17.
Lerner DN, Choi SS, Zalzal GH, Johnson DL. Intracranial complications of sinusitis in childhood. Ann Otol Rhinol Laryngol 1995;104(4 Pt 1):288–93. [CrossRef]
[Pubmed]

18.
Gadji N, Patel AJ, Gopinath SP. Open craniotomy for brain abscess: A forgotten experience? Surg Neurol Int 2013;4:34. [CrossRef]
[Pubmed]

19.
Elmallawany M, Ashry A, Alsawy MF. Endoscopic treatment of brain abscess. Surg Neurol Int 2021;12:36. [CrossRef]
[Pubmed]

20.
Moorthy RK, Rajshekhar V. Management of brain abscess: An overview. Neurosurg Focus 2008;24(6):E3. [CrossRef]
[Pubmed]

21.
Kawasaki H, Amano K, Kawamura H, et al. CT-guided stereotactic surgery of brain abscess. [Article in Japanese]. No Shinkei Geka 1991;19(2):143–8.
[Pubmed]

22.
Strowitzki M, Schwerdtfeger K, Steudel WI. Ultrasound-guided aspiration of brain abscesses through a single burr hole. Minim Invasive Neurosurg 2001;44(3):135–40. [CrossRef]
[Pubmed]

23.
Ke J, Tan S, Du YL, Ma FR. Successful treatment with ultrasound-guided aspiration of otogenic brain abscess with transmastoid approach. Chin Med J (Engl) 2020;133(10):1242–4. [CrossRef]
[Pubmed]

24.
Park HK, Kim YS, Oh SH, Lee HJ. Successful treatment with ultrasound-guided aspiration of intractable methicillin-resistant Staphylococcus aureus brain abscess in an extremely low birth weight infant. Pediatr Neurosurg 2015;50(4):210–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Sunday PU Nkwerem - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jude-Kennedy C Emejulu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Eric Okechukwu Umeh - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Chijioke C Umeokafor - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ofodile C Ekweogwu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Raphael C Nwosu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Sunday PU Nkwerem et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.