|
Case Report
Femoral intraosseous lipoma: Case report
1 Department of Radiology, Oncology National Institute, UHC Ibn Sina, Rabat, Morocco
2 Central Radiology Department, UHC Ibn Sina, Rabat, Morocco
Address correspondence to:
Sninate Sanae
MD, Resident in Radiology, Department of Radiology, Oncology National Institute, UHC Ibn Sina, Rabat,
Morocco
Message to Corresponding Author
Article ID: 101197Z01SS2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sanae S, Ayman EF, Youssef O, Hounayda J, Rachida L, Ittimade N. Femoral intraosseous lipoma: Case report. Int J Case Rep Images 2021;12:101197Z01SS2021.ABSTRACT
Introduction: Intraosseous lipoma is an extremely rare lesion that represents no more than 0.1% of all bone tumors. It is often misdiagnosed, unlike other benign bone lesions. With the combination of radiography, computed tomography (CT) and magnetic resonance imaging (MRI), the diagnosis can be done without histological confirmation.
Case Report: A 42-year-old man presented with a history of progressive left femoral pain radiating to his buttock and benefited from plain radiographs of the left hip showed a lytic lesion containing a central calcification and surrounded by sclerotic margins in the intertrochanteric region of the proximal femur. The patient underwent further evaluation with CT and MRI. Based on the results to the MRI and CT scan, intraosseous lipoma was confirmed and the need for further diagnostic tests has been eliminated.
Conclusion: We reported a rare case of symptomatic intraosseous lipoma of the femoral bone, which was difficult to diagnose on only plain radiographs. This showed the interest of MRI in the elimination of differential diagnosis and the confirmation of intraosseous lipoma
Keywords: Bone tumor, Imaging, Intraosseous lipoma
Introduction
Intraosseous lipoma is an uncommon benign bone tumor. The first case of intraosseous lipoma was reported by Brault in 1868 [1]. With an ever increasing use of cross-sectional imaging in the diagnostics of the musculoskeletal system, and especially of magnetic resonance imaging (MRI), the detection rate of those lesions has increased [2]. The aim of this work was to present a case of intraosseous lipoma of left intertrochanteric region of the proximal femur revealed by pain and to review the literature concerning this rare pathology.
Case Report
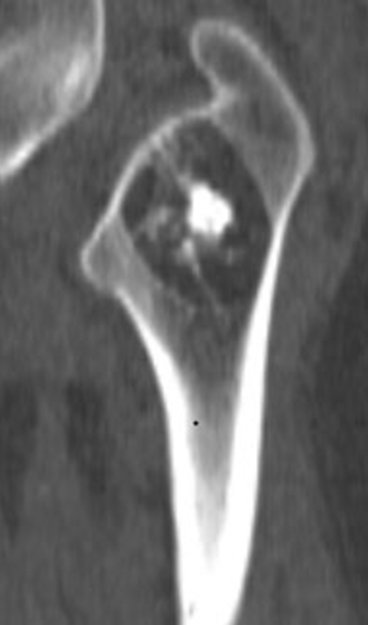
A 42-year-old man presented with a history of progressive left femoral pain radiating to his buttock. He reported worsening symptoms when walking for prolonged periods of time or playing sport. On clinical examination, he had no swelling, no tenderness, nor limitation of movement. Plain radiographs of the left hip showed a lytic lesion containing a central calcification and surrounded by sclerotic margins in the intertrochanteric region of the proximal femur (Figure 1). Axial CT scan reveals intraosseous well defined fat density lesion containing central calcification with sclerotic margins (Figure 2).
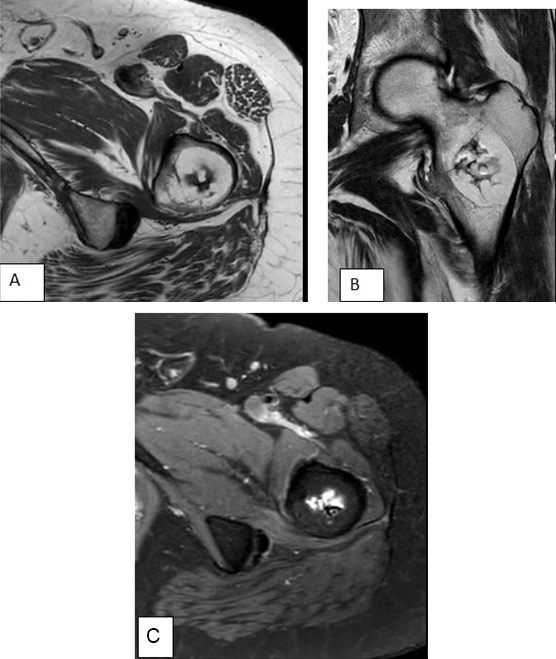
For further study, an MRI of the left hip was performed, axial MRI, T1-weighted (A), coronal T2-weighted (B), and axial T2-weighted images with fat suppression (C) showed in the intertrochanteric region of the proximal femur a hyperintense signal in the periphery’s lesion on T1-T2 weighted images, suppressed in the short tau inversion recovery (STIR) sequence corresponding to the fat, while the central part contains a space filled with fluid (low on T1, high on T2) and irregular internal low-signal-intensity area corresponding to dystrophic calcification (Figure 3). Based on the MRI results, the intraosseous lipoma was confirmed, and no other investigations were required.
Discussion
Intraosseous lipoma is one of the scarcest benign primary tumors of bone, with an incidence of less than one in 1000 cases [3]. There is no age predilection and both men and women are equally affected [1]. Recently the prevalence of these tumors has been increased, because it is usually asymptomatic and has been misdiagnosed with other primary bone tumors [4]. As symptoms occur, they are manifested by pain, swelling, and tenderness. Although intraosseous lipoma is considered as a benign bone lesion, Milgram has reported four cases of intraosseous lipoma transformed into malignant bone lesions [5].
The fatty components of intraosseous lipomas may display varying degrees of involution and necrosis, based on these characteristics. Milgram proposed three categories: Stage 1 sharply delineated, viable lipomas with homogeneous fat content, in stage 2: predominantly fatty lesions with central necroses, calcifications, or ossifications, in stage 3: heterogeneous, fat-containing lesions with multiple necroses, cystic transformations, wall sclerosis, and extensive calcifications or ossifications [1].
Regarding the case of this study, it is a stage 3 intraosseous lipoma since the lesion contains fat, dystrophic calcification as well as cystic spaces. The etiology of intraosseous lipoma is unknown; many theories were considered: a secondary posttraumatic bone reaction; fatty bone infarct with metaplasia; infection and tumor etiology because it is a benign tumor [5],[6].
It affects long bones, lipomas are most frequently found in metaphyseal and epiphyseal rather than in the diaphyseal region, the proximal portion of the femur, fibula, and calcaneus are most frequently affected. Tibia, distal portion of the femur, the vertebral bodies, the skull, the jaw, and the ribs which may also be affected [3].
The radiographic appearance of intraosseous lipomas is usually uncharacteristic and has a broad differential diagnosis which includes many benign bone lesions namely non-ossifying fibroma, fibrous dysplasia, solitary cyst, giant-cell bone tumor, bone infarct, and cartilaginous tumors [7].
Intraosseous lipomas usually present as cystic lesions with an increased radiolucency, surrounded by a sclerotic rim (74%) [2]. Lipomas located in the proximal femur may be surrounded by a relatively extensive area of sclerotization [8]. Lesions in the intertrochanteric area of the femur should be differentiated from liposclerosing myxofibrous tumor, a very scarce benign fibro-osseous lesion with mixed histology, which may contain components of lipoma [9].
The CT scan demonstration of intraosseous lipomas consists of a lytic lesion with distinct borders and a negative Hounsfield unit parallel to the adipose tissue. While irregularity of the bone cortex and marginal sclerosis surrounding the lesion are commonly observed [10]. Intraosseous lipoma presents on MRI as a lesion with a high signal intensity lesion on both T1 and T2-weighted images identical to that of adipose tissue that allows differentiation from other bone lesions [10].
Magnetic resonance imaging played an important role in confirming the diagnosis of this lesion prior to histopathological studies [11].
In the present case, the hyperintense signal on the T1 and T2 weighted images as well as the decrease in the signal in the fat removal image allowed the distinction between intraosseous lipoma and other bone lesions.
Currently, with the performance of CT and MRI in diagnosing intramedullary lipoma, the need for surgical biopsy for definitive diagnosis has become controversial [12].
It should be noted that asymptomatic lesions do not require surgical treatment and some of them may undergo spontaneous involution [13].
If a lesion or a malignant tumor followed by history, clinical and imaging findings, surgical treatment, and a biopsy should be performed. In our case, we did not perform a biopsy and a radiological follow-up was approached.
Conclusion
In this article, we reported a rare case of symptomatic intraosseous lipoma of the femoral bone, which was difficult to diagnose on only plain radiographs. This showed the interest of MRI in the elimination of differential diagnosis and the confirmation of intraosseous lipoma.
REFERENCES
1.
Milgram JW. Intraosseous lipomas. A clinicopathologic study of 66 cases. Clin Orthop Relat Res 1988;(231):277–302.
[Pubmed]

2.
Campbell RSD, Grainger AJ, Mangham DC, Beggs I, Teh J, Davies AM. Intraosseus lipoma: Report of 35 new cases and a review of the literature. Skeletal Radiol 2003;32(4):209–22. [CrossRef]
[Pubmed]

3.
4.
Yazdi HR, Rasouli B, Borhani A, Noorollahi MM. Intraosseous lipoma of the femor: Image findings. J Orthop Case Rep 2014;4(1):35–8. [CrossRef]
[Pubmed]

5.
Milgram JW. Malignant transformation in bone lipomas. Skeletal Radiol 1990;19(5):347–52. [CrossRef]
[Pubmed]

6.
Buckley SL, Burkus JK. Intraosseous lipoma of the ilium. A case report. Clin Orthop Relat Res 1988;(228):297–301.
[Pubmed]

7.
8.
Milgram JW. Intraosseous lipomas with reactive ossification in the proximal femur. Report of eight cases. Skeletal Radiol 1981;7(1):1–13. [CrossRef]
[Pubmed]

9.
Ragsdale BD. Polymorphic fibro-osseous lesions of bone: An almost site-specific diagnostic problem of the proximal femur. Hum Pathol 1993;24(5):505–12. [CrossRef]
[Pubmed]

10.
11.
Blacksin MF, Ende N, Benevenia J. Magnetic resonance imaging of intraosseous lipomas: A radiologic-pathologic correlation. Skeletal Radiol 1995;24(1):37–41. [CrossRef]
[Pubmed]

12.
Dooms GC, Hricak H, Sollitto RA, Higgins CB. Lipomatous tumors and tumors with fatty component: MR imaging potential and comparison of MR and CT results. Radiology 1985;157(2):479–83. [CrossRef]
[Pubmed]

13.
Bagatur AE, Yalcinkaya M, Dogan A, Gur S, Mumcuoglu E, Albayrak M. Surgery is not always necessary in intraosseous lipoma. Orthopedics 2010;33(5).
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Sninate Sanae - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
El Farouki Ayman - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Omor Youssef - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jerguigue Hounayda - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Latib Rachida - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nassar Ittimade - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Sninate Sanae et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.