|
Case Report
Necrotizing lung infections: Case report and review of the literature
1 David Geffen School of Medicine at University of California, Los Angeles (UCLA), Los Angeles, California, USA
Address correspondence to:
Ryan G Aronin
Internal Medicine, 100 UCLA Medical Plaza, Suite 490, Los Angeles, California 90095,
USA
Message to Corresponding Author
Article ID: 101120Z01RA2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Aronin RG, Park KW, Hoque A. Necrotizing lung infections: Case report and review of the literature. Int J Case Rep Images 2020;11:101120Z01RA2020.ABSTRACT
Introduction: Necrotizing lung infections represent a wide spectrum of disease of varying severities. The etiology is numerous, but mostly results from aspiration. Definitive diagnosis of necrotizing lung infections is radiographic, but can often be difficult to distinguish between necrotizing pneumonia and pulmonary gangrene. While the backbone of therapy involves antibiotics, optimal timing of surgery for advanced disease is poorly documented and unclear in the literature.
Case Report: We recently cared for a 50-year-old male who presented with and was subsequently admitted for treatment for necrotizing pneumonia.
Conclusion: Medical management with antibiotics remain the backbone of treatment for necrotizing pneumonia. Surgical intervention remains reserved for treatment failure or advanced necrotizing disease.
Keywords: Abscess, Lung, Necrotizing pneumonia
Introduction
Lower respiratory diseases are the leading cause of morbidity and mortality worldwide [1]. Necrotizing lung infections constitute a wide spectrum of disease of varying severity from lung abscesses to necrotizing pneumonia to pulmonary gangrene. These necrotizing infections are a sequela of pneumonia with indistinguishable features on onset, but have vastly different management patterns and clinical presentations [2]. In this case report, we aim to provide a comprehensive literature review on the etiology, presentation, and treatment for necrotizing lung infections.
Case Report
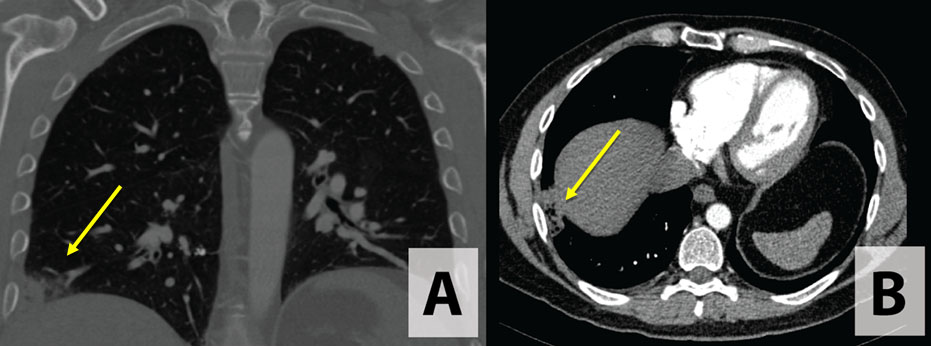
A 50-year-old non-smoking male history of basal cell carcinoma (BCC) status post-excision and gastroesophageal reflux disease (GERD) presented to urgent care with fatigue, shortness of breath (SOB), and right shoulder pain for one day. The patient was prescribed diazepam and a muscle relaxant for shoulder pain. Chest X-ray (CXR) noted a small pleural effusion on right lower lobe, and the patient was prescribed prednisone (six day course) with instructions for follow-up. Four days following this visit, the patient was seen by his primary care physician describing SOB, fatigue, and loss of appetite. The pain was noted to be intermittent and pleuritic. The patient denied any related fever, myalgia, headache, sick contacts, or hemoptysis. He described recently worsening GERD with nighttime awakenings with a sour taste in the back of his throat. As labs revealed elevated D-dimer and repeat CXR noted an ill-defined wedge like opacity in the right lower lobe (Figure 1), computed tomography (CT) chest with contrast was performed. Computed tomography chest revealed a 4 × 1.4 cm collection of fluid and gas at the lateral segment of the right lower lobe with surrounding stranding and edema (Figure 2). Differential diagnosis considered caseating abscess or necrotic tumor. The patient denied coughing, recent travel, no significant occupational, recreational exposures, or sick contacts.
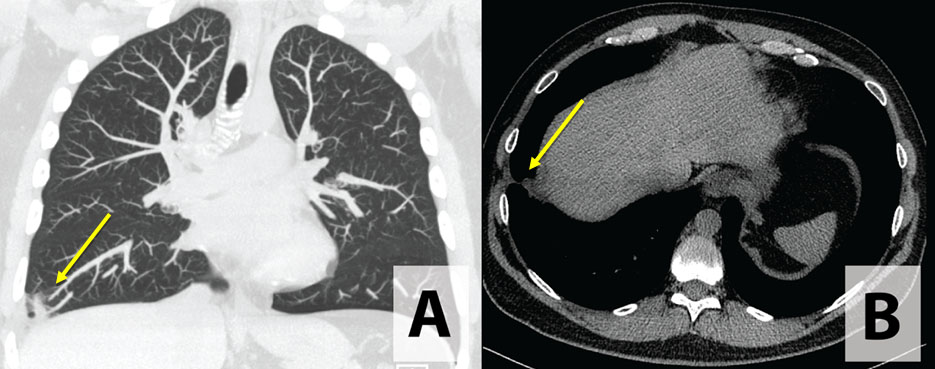
The patient was subsequently admitted, received intravenous (IV) ampicillin-sulbactam, and referred to Interventional Radiology and Pulmonology. Microbiologic workup included acid-fast bacilli (AFB) × 3, tuberculosis polymerase chain reaction (PCR) × 3, bacterial sputum culture, and other infectious workup including cryptococcal antigen, Histoplasma antigen, HIV, Coccidiosis, Aspergillus antigen, and quantiferon-gold. Pulmonary medicine felt the patient had necrotizing pneumonia secondary to recurrent aspiration events. No drainage was recommended, and instead the patient was discharged with an extended course of antibiotics with four weeks of amoxicillin/clavulanic acid (Augmentin®) and azithromycin for atypical coverage. Four weeks following discharge, repeat CT with contrast revealed interval resolution of the consolidation and abscess with mild scarring remaining (Figure 3).
Discussion
The etiology of necrotizing infections is numerous, but most commonly arises from aspiration [3]. Common risk factors for aspiration include, but are not limited to GERD, sinusitis, loss of consciousness, intubation, and alcoholism [3]. Secondary sources of necrotizing infections include bronchial obstructions, HIV, neoplasms, hematological infections, and pre-existing lung conditions. Our patient had GERD that may have contributed to the development of the lung abscess, but otherwise had no significant past medical history. Interestingly, prior to the widespread use of antibiotics, abscesses were predominantly caused by a single organism, but are now mostly polymicrobial [4]. In the United States and Europe, the most common organisms responsible for community-acquired abscesses are anaerobes and Streptococcus species that typically colonize the oral cavity. However, in Taiwan and parts of eastern Asia, Klebsiella pneumoniae is the most common organism for community-acquired abscesses, and special care must be taken for appropriate antibiotic coverage in this population [4].
The clinical symptoms of necrotizing lung infections vary significantly as the disease begins to develop. Simple lung abscesses typically develop 7–14 days after pneumonitis due to tissue necrosis, and have an indolent course. Patients may present with bitter taste, weight loss, fever, night sweats, and pleuritic pain that fail to resolve with outpatient treatment [2],[5]. Furthermore, the classification of lung abscesses can be divided into acute (<6 weeks) and chronic (>6 weeks). However, patients with necrotizing pneumonia or pulmonary gangrene typically present with more severe symptoms including sepsis and respiratory failure requiring ventilator support [2]. Pulmonary gangrene is often distinguished from necrotizing pneumonia by a more diffuse area of necrosis and large vessel thrombosis, which is thought to play a pathological role in the development of gangrene [2].
Radiographically, CXR will demonstrate an isolated cavity containing an air fluid level for a simple abscess. For necrotizing pneumonia and pulmonary gangrene, CXRs may demonstrate bulging fissures due to inflammation and more diffuse involvement, but CT thorax is recommended for further evaluation. Computed tomography thorax of necrotizing pneumonia may initially present with multiple small cavities [6]. In our case, the patient presented with an isolated 4 cm abscess at the right lower lobe. However, there was no evidence of necrosis evident of necrotizing pneumonia or pulmonary gangrene.
The backbone of management for necrotizing lung infections is antibiotics. On admission, patients are often started on empiric antibiotics while the offending microbial agent is identified [2],[7]. For lung abscesses due to anaerobic and streptococcal infections, patients are given oral amoxicillin/clavulanic acid. Atypical coverage for organisms with azithromycin is also often given. Currently, there is no consensus on the duration of treatment for simple lung abscesses, but is usually recommended around 6–8 weeks for treatment based on the clinical and radiographic response of the patient. Surgical treatment of lung abscesses including chest tube placement, resection, and endoscopic drainage is only required when medical management fails. Previous studies have found prognosticators for medical failure to include large cavity size (>8 cm), large pleural collections, and resistant organisms [7]. As our patient had no significant risk factors to suggest medical treatment failure and presented with a well-defined abscess, he was stabilized and discharged on four weeks on antibiotics with full resolution seen on CT at four weeks follow-up. However, if our patient had any of these prognosticators for medical treatment failure, surgical treatment may be considered upfront if no improvement is seen. In contrast to lung abscesses, surgical involvement is warranted in the management of necrotizing pneumonia and pulmonary gangrene. However, the optimal timing of surgery for resection is unclear and poorly documented in the literature [6],[8].
Conclusion
Necrotizing lung infections encompass a wide spectrum of disease of varying severities. Most patients are diagnosed following treatment failure for pneumonia with usual courses of outpatient antibiotics. Medical management with antibiotics remains the backbone of treatment for necrotizing lung infections with surgical intervention reserved for treatment failure or advanced forms of necrotizing disease including necrotizing pneumonia and pulmonary gangrene.
REFERENCES
1.
GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis 2018;18(11):1191–210. [CrossRef]
[Pubmed]

2.
Chatha N, Fortin D, Bosma KJ. Management of necrotizing pneumonia and pulmonary gangrene: A case series and review of the literature. Can Respir J 2014;21(4):239–45. [CrossRef]
[Pubmed]

3.
Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med 2015;3(13):183. [CrossRef]
[Pubmed]

4.
Takayanagi N, Kagiyama N, Ishiguro T, Tokunaga D, Sugita Y. Etiology and outcome of community-acquired lung abscess. Respiration 2010;80(2):98–105. [CrossRef]
[Pubmed]

5.
Sanders CV, Hanna BJ, Lewis AC. Metronidazole in the treatment of anaerobic infections. Am Rev Respir Dis 1979;120(2):337–43.
[Pubmed]

6.
Reimel BA, Krishnadasen B, Cuschieri J, Klein MB, Gross J, Karmy-Jones R. Surgical management of acute necrotizing lung infections. Can Respir J 2006;13(7):369–73. [CrossRef]
[Pubmed]

7.
8.
Krishnadasan B, Sherbin VL, Vallières E, Karmy-Jones R. Surgical management of lung gangrene. Can Respir J 2000;7(5):401–4. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Ryan G Aronin - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ki Wan Park - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Asraful Hoque - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionKi Wan Park is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Ryan G Aronin et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.