|
Case Series
The use of microneedling associated to photobiomodulation in the treatment of male androgenetic alopecia: Case series
1 Graduate Student, Postgraduate Program in Biophotonics Applied to Health Sciences, Universidade Nove de Julho (UNINOVE), São Paulo, Brazil
2 Postgraduate Program in Biophotonics Applied to Health Sciences, Universidade Nove de Julho (UNINOVE), São Paulo, Brazil
Address correspondence to:
Christiane Pavani
Programa de Pós-Graduação em Biofotônica Aplicada às Ciências da Saúde, Universidade Nove de Julho/UNINOVE, R. Vergueiro 235/249, CEP 01504-001, São Paulo,
Brazil
Message to Corresponding Author
Article ID: 101079Z01NP2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Pedroso NM, Mota LR, Pavani C. The use of microneedling associated to photobiomodulation in the treatment of male androgenetic alopecia: Case series. Int J Case Rep Images 2019;10:101079Z01NP2019.ABSTRACT
Introduction: Androgenetic alopecia (AA) is a pathology associated to hormonal imbalance and affects men and women causing reduction and/or absence of hair in a particular region of the scalp. Some of the pharmacological treatments available in the market are inefficient and/or present risks and contraindications. Here, a combination of two minimally invasive techniques (photobiomodulation and microneedling) was proposed as a four-week treatment protocol in the treatment of male AA within a case series.
Case Series: The one-month treatment was performed in three men with AA, being 12 applications of photobiomodulation (three times a week) using low intensity laser (4 J per point, 40 seconds, 660 nm, 10 mW) and two microneedling sessions with a 15-day interval between them. The main outcome was the density of hair strands per square centimeter (n/cm2). The analysis was performed through a dermatoscope that registered scalp images and software was used to count the number of strands. The images were recorded before the beginning of the treatment, after the sixth session (day 15), after the twelfth session (day 30), and thirty days after the end of the treatment (day 60). After four weeks of the end of the treatment, the hair count increased from 111.1 to 140.6 hair/cm2 (pooled data from all patients). The patients reported reduced dissatisfaction with hair loss after the end of the treatment.
Conclusion: The association of microneedling with photobiomodulation is a promising alternative for the treatment of male AA.
Keywords: Alopecia, Low intensity laser, Male androgenetic alopecia, Microneedling
Introduction
Androgenetic alopecia (AA) is related to the action of dihydrotestosterone (DHT), a testosterone metabolite and it is characterized by miniaturization of the hair, reducing of the anagen and increasing the telogen phase [1],[2]. The AA is present both in men and women, and it is the most common type of alopecia, which is a multifactorial pathology related to hereditary factors, hormonal changes, nutritional deficiencies, autoimmunity, stress, and others [3],[4]. There are different types of treatments for AA: topical, systemic, and surgical treatments [5]. Current treatments have some side effects and high cost [6]. Some drugs, such as finasteride and minoxidil, present side effects, such as dryness, erythema, skin irritation and allergic contact dermatitis, erectile dysfunction, and impotence [7]. Thus, noninvasive techniques, such as microneedling and photobiomodulation (PBM), have emerging as interesting alternatives in the treatment of AA for those who are not willing to conventional treatments with medicines or hair transplants [8]. The microneedling generates small roles in the cutaneous surface increasing the permeation of cosmetics and active ingredients, and also triggers the release of growth factors and neovascularization [9]. In the treatment of AA, induces the expression of Wnt proteins, which stimulate the stem cells from dermal papilla, inducing hair growth [10]. Photobiomodulation in the treatment of AA acts by increasing the production of energy in the form of adenosine triphosphate, increasing cell metabolism and hair growth [11]. These two minimally invasive techniques have shown to be promising, however, there are no reports regarding their combination. The objective of this series was to evaluate the efficacy of the combined protocol of microneedling associated to PBM in the treatment of male AA.
CASE SERIES
This study was designed following the Declaration of Helsinki. The procedures used within this study were approved by the Research Ethics Committee of the Nove de Julho University on August 20, 2018 with acceptance number 2.831.378. The informed consent form was filled and signed by the participants of the study. During the enrollment, the participants answered to an anamnesis and were evaluated by the researcher. The information was used to check the inclusion/exclusion criteria. The inclusion criteria were male patients, above 25 years old and presenting AA. Exclusion criteria were dandruff, dermatitis, and any type of scalp infections, lesions, or inflammations; skin cancer lesions; use of anticoagulants, corticosteroids, or anti-inflammatories; oral use of isotretinoin; use of oral or topical substances for hair treatment; use of medicines that increase skin photosensitivity; psoriasis; keratosis; diabetes mellitus; and warts. The treatment was performed during 4 weeks, being 12 applications of PBM, 3 times a week and 2 sessions of microneedling with interval of 15 days. In the first and seventh sessions, patients received topical anesthetic with 4% lidocaine cream (Dermomax, Aché Laboratory, São Paulo, Brazil) 30 minutes before the procedure in the region to be treated. Following the cream was withdrawn and region hygienized with 0.5% aqueous chlorhexidine solution. Then, the 0.5 mm roller (DermaRoller System, China) was applied, with a maximum of 10 passes per quadrant in all directions (horizontal, vertical, and diagonal). Then, the PBM with laser therapy EC (DMC, Florida, USA) was applied in the region affected by alopecia, at points 1 cm apart, homogeneously distributed throughout the area (660 nm, 100 mW, 40 seconds, 4 J per point). At all the other sessions (only PBM application), the treated region was hygienized with 0.5% aqueous chlorhexidine solution and PBM was applied according to the previous description.
A dermatoscope (BW-400X, Duratool, Taiwan) was used to record images of the scalp before (D0), after the sixth session (D15), after twelfth session (end of treatment, D30), and 30 days after the end of treatment (follow-up, D60), as presented at the flow chart (Figure 1). Ten images from each participant were recorded at all time points, evaluating all the area affected by alopecia. Image J software (NIH) was used to count the follicles containing hair strands per square centimeter (n/cm2) in each image. The Shapiro–Wilk test was used to evaluate the normality of the data. As the data were nonparametric, they were analyzed by the Friedman test, followed by a two-by-two comparison using the Wilcoxon test using GraphPad Prism software. Before receiving the first intervention (D0) and 30 days after the end of treatment (D60), the patients were asked regarding their dissatisfaction/discomfort with the dysfunction through a scale ranging from 0 to 10, where 0 meant no discomfort and 10 high discomfort (Figure 1).
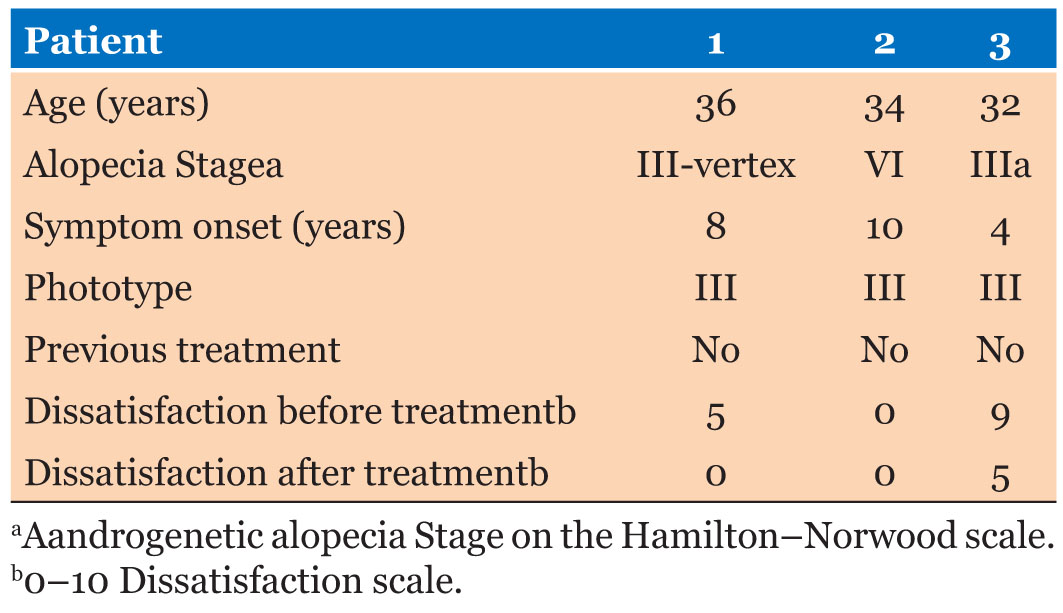
The patients, who participated in this study, were around 34 years old. The alopecia Stage was variable from III to VI by the Hamilton–Norwood scale while the symptoms started 4 to 10 years ago. From all patients, only patient 2 reported absence of dissatisfaction with the hair loss before the treatment started. Patients 1 and 3 presented reduced dissatisfaction after the end of the treatment. The detailed information is presented in Table 1.
All patients presented hair loss at the parietal and temporal region, and also at the vertex. The photos presented at Figure 2 showed the increase in hair density at the vertex region of the patients 1 and 2, while no difference was observed in patient 3, when comparing before treatment and at the follow-up (Figure 2A and Figure 2B, Figure 2G and Figure 2H, Figure 2M and Figure 2N). The scalp photos showed a gradual increase in the number of strands when comparing before treatment (D0), after the sixth session (D15), on the last day of treatment (D30), and 30 days after the treatment finished (D60) (Figure 2C–F for patient 1, I–L for patient 2, and O–R for patient 3). Although this parameter has not been determined, it is also possible to observe in the photos, the increase in the thickness of the strands during the treatment (Figure 2).
The counts of the number of hair strands at 10 photos in each of the analysis periods for each patient showed a gradual increase in the total number of wires (Figure 3). A statistically significant difference (p < 0.05) was observed in the number of wires after 60 days of treatment compared to day 0 in patient 1 (Figure 3A) and patient 2 (Figure 3B). No difference was observed in patient 3 (Figure 3C) when comparing day 0 and day 60 while a decrease in the number of strands (n/cm2) at day 30. The pool of data of the three patients exhibited a statistically significant increase in the number of strands per area (n/cm2) at the follow-up (day 60), 30 days after the end of the treatment (Figure 3D).
Discussion
The use of PBM as a therapy for AA has shown to be a safe option for the treatment of AA, promoting the increase in hair count without side effects and upregulation of proteins which are involved in the promotion of hair growth and reversing of miniaturization observed in AA patients [11],[12]. The results of this study corroborate with Jimenez et al. (2014) which evaluated the efficacy of HairMax Laser Comb device in increasing capillary density in men and women who received treatment 3 times a week for 26 weeks, the results showed increased capillary density in both sexes, with absence of side effects [13]. Suchonwanit et al. (2018) performed a study similar to Jimenez et al.’s, evaluating effectiveness of PBM in the treatment of AA using a helmet-shaped device. Forty individuals of both sexes underwent 24 weeks of treatment and the device proved to be effective with minimal side effects [14]. However, these studies were effective (and showed statistically difference in hair count per area) in more than 20 weeks of treatment. The combination of microneedling and PBM used here was effective in promoting hair regrowth in a 30 days (four weeks) treatment, being the results statistically significant 30 days after the protocol was performed.
The increase in hair count from 137.3 hair/cm2 on baseline to 145.1 hair/cm2 at the end of 14 weeks of PBM therapy (655 and 780 nm, 10 minutes daily, no radiant exposure was mentioned) was reported before, that is, a 6% increase in hair density [15]. Here, after four weeks of the combined treatment (PBM + microneedling) the hair count increased from 111.1 to 140.6 hair/cm2 (pooled data), a 26% increase in hair density, showing that this is a promising protocol for AA treatment.
Microneedling promotes an inflammatory process and acts on the release of important growth factors in follicle stimulation [10]. Arsie Contin et al. reported in their study that there is a need for the use of minoxidil associated with microneedling for better results [6]. Jha et al. performed a clinical study in patients suffering from AA comparing the use of minoxidil alone, associated to platelet rich plasma (PRP) and minoxidil associated to microneedling and PRP. The results showed that the group which received the combination of the three therapies presented better results with respect to hair regrowth indicating that the use of combination therapies bring greater results in the treatment of AA [16]. Here, we could observe that the use of microneedling associated to PBM was effective for treatment of this type of alopecia. Besides, the combined treatment showed to be more effective than the single ones (PBM or microneedling) by the data found in literature [15],[16]. The clinical protocol used here is a low cost one and has few contraindications and adverse effects in relation to other treatment options, making it an appropriate resource for the professional treating alopecia. Further studies, randomized and double blind clinical trials are needed to prove the effectivity of this combined protocol regarding the isolated ones. This case report inspired our group to develop a randomized clinical trial based upon this combination of therapies which is already recruiting [17].
Conclusion
The pooled data from the three patients showed 26% increase in hair density after the four weeks protocol of microneedling associated to PBM, showing that this is a promising and effective protocol.
REFERENCES
1.
Kaufman KD. Androgens and alopecia. Mol Cell Endocrinol 2002;198(1–2):89–95. [CrossRef]
[Pubmed]

2.
Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol 1977;97(3):247–54. [CrossRef]
[Pubmed]

3.
Norwood OT. Male pattern baldness: Classification and incidence. South Med J 1975;68(11):1359–65. [CrossRef]
[Pubmed]

4.
Yip L, Rufaut N, Sinclair R. Role of genetics and sex steroid hormones in male androgenetic alopecia and female pattern hair loss: An update of what we now know. Australas J Dermatol 2011;52(2):81–8. [CrossRef]
[Pubmed]

5.
Yildiz BO. Diagnosis of hyperandrogenism: Clinical criteria. Best Pract Res Clin Endocrinol Metab 2006;20(2):167–76. [CrossRef]
[Pubmed]

6.
7.
Dhariwala MY, Ravikumar P. An overview of herbal alternatives in androgenetic alopecia. J Cosmet Dermatol 2019;18(4):966–75. [CrossRef]
[Pubmed]

8.
Kim H, Choi JW, Kim JY, Shin JW, Lee SJ, Huh CH. Low-level light therapy for androgenetic alopecia: A 24-week, randomized, double-blind, sham device-controlled multicenter trial. Dermatol Surg 2013;39(8):1177–83. [CrossRef]
[Pubmed]

9.
Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev 2004;56(5):603–18. [CrossRef]
[Pubmed]

10.
Fertig RM, Gamret AC, Cervantes J, Tosti A. Microneedling for the treatment of hair loss? J Eur Acad Dermatol Venereol 2018;32(4):564–9. [CrossRef]
[Pubmed]

11.
Darwin E, Heyes A, Hirt PA, Wikramanayake TC, Jimenez JJ. Low-level laser therapy for the treatment of androgenic alopecia: A review. Lasers Med Sci 2018;33(2):425–34. [CrossRef]
[Pubmed]

12.
Panchaprateep R, Pisitkun T, Kalpongnukul N. Quantitative proteomic analysis of dermal papilla from male androgenetic alopecia comparing before and after treatment with low-level laser therapy. Lasers Surg Med 2019;51(7):600–8. [CrossRef]
[Pubmed]

13.
Jimenez JJ, Wikramanayake TC, Bergfeld W, et al. Efficacy and safety of a low-level laser device in the treatment of male and female pattern hair loss: A multicenter, randomized, sham device-controlled, double-blind study. Am J Clin Dermatol 2014;15(2):115–27. [CrossRef]
[Pubmed]

14.
Suchonwanit P, Chalermroj N, Khunkhet S. Low-level laser therapy for the treatment of androgenetic alopecia in Thai men and women: A 24-week, randomized, double-blind, sham device-controlled trial. Lasers Med Sci 2019;34(6):1107–14. [CrossRef]
[Pubmed]

15.
Kim SS, Park MW, Lee CJ. Phototherapy of androgenetic alopecia with low level narrow band 655-nm red light and 780-nm infrared light. J Am Acad Dermatol 2007;56(2 Suppl 2):AB112. [CrossRef]

16.
Jha AK, Vinay K, Zeeshan M, Roy PK, Chaudhary RKP, Priya A. Platelet-rich plasma and microneedling improves hair growth in patients ofandrogenetic alopecia when used as an adjuvant to minoxidil. J Cosmet Dermatol 2019;18(5):1330–35. [CrossRef]
[Pubmed]

17.
da Silveira SP, Moita SRU, da Silva SV, Rodrigues MFSD, da Silva DFT, Pavani C. The role of photobiomodulation when associated with microneedling in female pattern hair loss: A randomized, double blind, parallel group, three arm, clinical study protocol. Medicine (Baltimore) 2019;98(12):e14938. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
The authors acknowledge the University Nove de Julho for the institutional structure of the Ambulatory for patient care. CP thanks Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for the Research Fellowship (grant # 311737/2017-0).
Author ContributionsNayá Madeira Pedroso - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lidiane Rocha Mota - Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Christiane Pavani - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Nayá Madeira Pedroso et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.