|
Case Report
From diagnosis to treatment of post-polio syndrome: A case study
1 Medical student at Iguaçu University - UNIG/RJ, Nova Iguaçu - RJ, Brazil
2 Medical student at Iguaçu University, Iguaçu University - UNIG/RJ, Nova Iguaçu - RJ, Brazil
3 Physician, Neurologist, Adjunct Professor of Medicine at Universidade Iguaçu - UNIG/ Nova Iguaçu, RJ, Brazil
4 Department of Neurology of Hospital Geral de Nova Iguaçu, PhD student in Neurology at the Federal University of the State of Rio de Janeiro - UNIRIO, Adjunct Professor of Medicine at Iguaçu University - UNIG/Nova Iguaçu, RJ, Brazil
5 Professor of Neurology - Universidade Iguaçu - UNIG-RJ, Nova Iguaçu - RJ; Physician of the Neurology Service of Nova Iguaçu General Hospital, Nova Iguaçu, RJ, Brazil
6 Physician, Neurologist, State University of Rio de Janeiro - UERJ, Rio de Janeiro, RJ, Brazil
Address correspondence to:
Antonio Marcos da Silva Catharino
Rua Gavião Peixoto 70, Room 811, CEP 24.2230-100, Icaraí, Niterói-RJ,
Brazil
Message to Corresponding Author
Article ID: 101384Z01DP2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Pereira DA, Santos YFMC, Neves MAO, da Silva Catharino AM, Martins GC, Davidovich ER. From diagnosis to treatment of post-polio syndrome: A case study. Int J Case Rep Images 2023;14(1):61–65.ABSTRACT
Introduction: Acute anterior poliomyelitis (AAP) can affect people of any age, despite being uncommon before six months. The viral invasion destroys the lower motor neurons of the spinal cord, brain, and brainstem. As a result, it leads to partial or complete flaccid and asymmetrical paralysis of the lower limb and spine muscles. Big names like Frida Kahlo and US President Franklin D Roosevelt were diagnosed with polio.
Case Report: We present the case of a patient with AAP diagnosed at two years of age. As an adult, he gave osteomyoarticular sequelae, insomnia, new central (adynamia), peripheral fatigue, cold intolerance, joint and neuropathic pain. The patient received a clinical diagnosis of post-polio syndrome (PPS) after fulfilling Dalakas criteria. The physical examination showed some hallmarks of AAP, in addition to those primarily affected by PPS.
Conclusion: Post-polio syndrome is a disorder characterized by new neuromuscular deficits that present years after the resolution of polio infection. However, far beyond the physical pain, the psychosocial impact is staggering. Therefore, in addition to surgical intervention and physical therapy, attention should be paid to the psychological follow-up of this patient, who is most often elderly.
Keywords: Acute poliomyelitis, Poliomyelitis, Post-polio syndrome
Introduction
Acute anterior poliomyelitis (AAP), infantile palsy, Heine-Medin disease, and poliomyelitis are additional names for the same illness [1],[2]. However, it is crucial to stress that infantile paralysis can affect people of any age, despite being uncommon before six months [3]. Additionally, reports of this illness date back to antiquity, and at the end of the 19th century, epidemics caused it to become a public health concern [2].
The lower motor neurons of the spinal cord, brain, and brainstem are destroyed by the viral invasion that causes AAP, a disease with a viral etiology caused by three types of poliovirus (I, II, and II) of the enterovirus genus (sensory neurons are spared) [1],[2]. As a result, it leads to partial or complete flaccid and asymmetrical paralysis of the lower limb and spine muscles [1],[3],[4].
Clinically, AAP can present as asymptomatic, abortive, non-paralytic, or paralytic, with the last two clinical manifestations occurring less frequently. Typically, the person exhibits no symptoms (asymptomatic infection) or only mild symptoms like fever, malaise, nausea, vomiting, constipation, abdominal pain, and meningeal signs (non-paralytic). Along with these symptoms, it is also possible to notice convulsions, drowsiness, irritation, and muscle pain in the neck and trunk [1],[3]. On the other hand, the paralytic form entails flaccid, abrupt, and asymmetrical paralysis, the reduction or elimination of deep reflexes in the paralyzed area, and the preservation of sensitivity and areflexia in the affected region [1],[2].
About the diagnosis of poliomyelitis, if it is done only clinically, it will not be enough. Therefore, laboratory confirmation is essential, and the gold standard is the isolation of the virus. This confirmation can be made from stool, oropharynx, and cerebrospinal fluid samples. Regarding the differential diagnosis, among the many that exist, we can mention diseases caused by other viruses (such as EV-71 and Coxsackie), Guillain–Barré syndrome, and anterior flaccid palsy (PFA) [1].
Famous names in recent history are examples of polio’s pain. Frida Kahlo caught polio in 1913, aged six, and spent several months in bed. In 1921, while on vacation with his family, Franklin Delano Roosevelt, then 39, developed symptoms and was later diagnosed with polio. In addition to physical pain and its limitations, psychological pain was a severe factor in life and consequently in the work of Frida Kahlo. Her right leg was visibly damaged, and trophic ulcers appeared. Roosevelt was the inspiration behind the nonprofit, which stood out by continuing to raise awareness of polio and money for research—financing a large portion of the study that resulted in the creation of the Salk and Sabin vaccines [5],[6],[7].
Post-polio syndrome (PPS) is a set of signs and symptoms that affect the nervous system in individuals who have had polio, usually after 15 years or more. A motor neuropathy fits the motor neuron disease (MND), these being lower motor neurons.
Post-polio syndrome is defined as the development of new muscle weakness and fatigue of the skeletal and bulbar innervation muscles, unrelated to other causes.
The pathophysiology behind PPS remains unclear but is likely multifactorial. Deterioration of neuromuscular functions, overuse of motor units, the general aging process, and inflammatory changes in the central nervous system and serum have all been proposed as possible explanations for the new symptoms. In addition, the late effects of poliomyelitis (including arthritis, tendonitis, muscle wasting, osteoporosis, and fracture), often a consequence of biomechanical changes, can mimic PPS or be amplified by PPS [8],[9].
Motor units gradually grow abnormally large, up to seven times their original size, making them incapable of supporting their metabolic rate. The time it takes from the acute infection to the onset of PPS symptoms can be up to three decades [9],[10]. Inflammatory modifications and increased expression of E2 synthetic pathway enzymes are also seen in skeletal muscle biopsies. The time it takes to go from an acute infection to the onset of PPS symptoms can be up to three decades [8],[11].
The main symptoms are pain, loss of strength, fatigue, tiredness, intolerance to cold, dysphagia, cognitive complaints, and depressive symptoms. Fatigue, tiredness, depression, and cognitive complaints were significantly more frequent in women [12].
The number of interventions, number of limbs affected, length of time required for gait recovery, and severity of sequelae after recovery from the primary infection all contribute to the severity of PPS. Therefore, a more severe acute infection may be linked to older age at disease onset, which could result in more severe sequelae. All of these elements could make PPS more likely to occur [12],[13].
Case Report
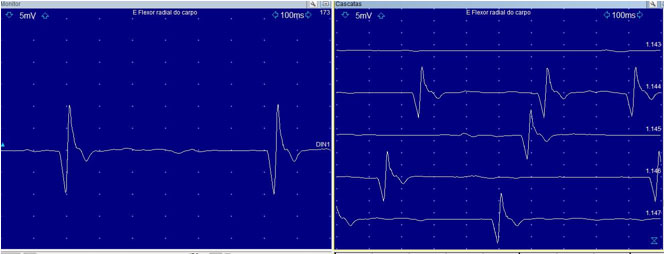
CEC, 47 years old, without comorbidities, reported that at the age of two, he had flaccid paralysis with subsequent hospitalization in an intensive care unit for two months. He had been diagnosed with previous acute poliomyelitis, with sequelae in the left side of the body (amyotrophy and areflexia) and osteo-myo-articular involvement (Figure 1, Figure 2, Figure 3). After about 20 years, insomnia, a new condition of central (dynamia) and peripheral fatigue began, cold intolerance, joint and neuropathic pain. The patient received a clinical diagnosis of PPS after fulfilling Dalakas criteria. Electroneuromyography was with chronic preganglionic involvement with chronic snowfall (Figure 4). Magnetic resonance imaging (MRI) of the thoracic and lumbar cervical spine: disc protrusions in several segments, but no reaction with the immersion of the clinical picture. Blood count was normal and no other clinical condition explains such a condition.
Discussion
It is noteworthy that the patient had physical and psychological characteristics of PPS, such as insomnia and cold intolerance [14]. Thus, they demonstrate pain in addition to the physical pain itself; for example, numerous reports of PPS have depression.
Some theories about the pathophysiology of PPS help to understand the patient’s musculoskeletal sequelae because, in addition to the damage to motor neurons by the virus, inflammatory changes in the central nervous system, the aging process itself, and even the excessive use of motor units throughout of years and decades can corroborate the syndrome.
Studies have not advanced much in the specific treatment of PPS, and physical therapy is still the most significant indication of treatment, accompanied by medications for analgesia and other patient demands. One of these demands is a psychological follow-up, as it is necessary to pay attention to the psychosocial damages of this syndrome. Physiotherapy aims to prevent overuse while focusing on increasing endurance [15],[16].
According to the severity of the AAP, the need for surgical interventions is already well established in the literature, and the patient did not have any previous surgery related, possibly indicating a picture of mild or moderate AAP. Thus, this report corroborates the theory that, regardless of the severity of AAP, there is a risk of PPS.
The pain of mechanical origin is predominant, mainly related to joint and muscle-tendon involvement. Many patients put extra weight on a limb previously thought to be disease-free so that new-onset weakness can affect these limbs [15],[17].
Although considerable changes are seen on electromyography and changes on MRI of the thoracic and lumbar cervical spine, the diagnosis of PPS is always clinical.
Conclusion
Post-polio syndrome is a disorder characterized by new neuromuscular deficits that present years after the resolution of polio infection. However, far beyond the physical pain, the psychosocial impact is staggering. Therefore, in addition to surgical interventions, and physical therapy, attention should be paid to the psychological follow-up of this patient, who is most often elderly.
REFERENCES
2.
Durante ALTC, Poz MRD. Global health and Brazilian health responsibility: The case of polio eradication. Saúde Debate 2014;38(100):129–38. [CrossRef]

3.
4.
Lima V, Fernanda F, Quadros AAJ, Oliveira ASB, Fontes SV, Fávero FM. Estudo retrospectivo do comportamento da força muscular em pacientes com Síndrome Pós-Poliomielite. Rev Neurocienc 2014;22(3):351–8. [CrossRef]

5.
Polioplace: A service of Post-polio Health International. Franklin Delano Roosevelt. [Available at: http://www.polioplace.org/people/franklin-delano-roosevelt#]

6.
Hart CW. Franklin Delano Roosevelt: A famous patient. J Relig Health 2014;53(4):1102–11. [CrossRef]
[Pubmed]

7.
Budrys V. Neurological deficits in the life and works of Frida Kahlo. Eur Neurol 2006;55(1):4–10. [CrossRef]
[Pubmed]

8.
Chu ECP, Lam KKW. Post-poliomyelitis syndrome. International Medical Case Reports Journal 2019;12:261–4. [CrossRef]

9.
Li Hi Shing S, Chipika RH, Finegan E, Murray D, Hardiman O, Bede P. Post-polio syndrome: More than just a lower motor neuron disease. Front Neurol 2019;10:773. [CrossRef]
[Pubmed]

10.
Bertolasi L, Danese A, Monaco S, Turri M, Borg K, Werhagen L. Polio patients in Northern Italy, a 50 year follow-up. Open Neurol J 2016;10:77–82. [CrossRef]
[Pubmed]

11.
Li Hi Shing S, Lope J, Chipika RH, Hardiman O, Bede P. Extra-motor manifestations in post-polio syndrome (PPS): Fatigue, cognitive symptoms and radiological features. Neurol Sci 2021;42(11):4569–81. [CrossRef]
[Pubmed]

12.
Sáinz MP, Pelayo R, Laxe S, Castaño B, Capdevilla E, Portell E. Describing post-polio syndrome. Neurologia (Engl Ed) 2022;37(5):346–54. [CrossRef]
[Pubmed]

13.
14.
Bruno RL, Frick NM. The psychology of polio as prelude to post-polio sequelae: Behavior modification and psychotherapy. Orthopedics 1991;14(11):1185–93. [CrossRef]
[Pubmed]

15.
García-Salgado A, Grande-Alonso M. Biobehavioural physiotherapy through telerehabilitation during the SARS-CoV-2 pandemic in a patient with post-polio syndrome and low back pain: A case report. Phys Ther Res 2021;24(3):295–303. [CrossRef]
[Pubmed]

16.
Amole M, Khouzam-Skelton N. Diagnosing post-polio syndrome in the elderly, a case report. Geriatrics (Basel) 2017;2(2):14. [CrossRef]
[Pubmed]

17.
Neves MAO, de Mello MP, dos Santos VV, et al. Post-poliomyelitis syndrome: Case report. Arq Neuropsiquiatr 2007;65(2B):528–31. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Daniel Antunes Pereira - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yasmin Faria Menezes Castro Santos - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marco Antônio Orsini Neves - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Antonio Marcos da Silva Catharino - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Gilberto Canedo Martins Jr - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Eduardo Rodrigues Davidovich - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Daniel Antunes Pereira et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.