|
Case Series
Cardiac and great vessels pseudoaneurysms and their challenging options of the management in children
1 Pediatric Cardiology Department, King Fahad Medical City-King Salman Heart Center, Riyadh, Saudi Arabia
Address correspondence to:
Ghada Shiekheldin M Abdullah
Pediatric Cardiology Department, King Fahad Medical City-King Salman Heart Center, P.O. Box 59046, Riyadh 11525,
Saudi Arabia
Message to Corresponding Author
Article ID: 101376Z01GA2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Abdullah GSM, Almoukirish A, Tagaldin M, Obaidan MB, Milad ES. Cardiac and great vessels pseudoaneurysms and their challenging options of the management in children. Int J Case Rep Images 2023;14(1):23–27.ABSTRACT
Introduction: Cardiac and great vessel pseudoaneurysms are often difficult to diagnose and might be easily missed. Delay in diagnosis and management may lead to serious event.
Case Series: We are presenting three cases with huge pseudoaneurysms. The clinical approach, diagnostic imaging, and challenging options of management were illustrated. The first case was 12 years old girl presented with clinical features of bacterial endocarditis; echocardiography showed multiple vegetations on mitral valve (MV). She underwent cardiac surgery with removal of vegetation and repair of MV. Three weeks later an echocardiogram revealed a large left ventricle (LV) lateral wall pseudoaneurysm. She underwent aneurysmectomy and repair of LV lateral wall. Second case, a 3 years old girl with history of fever for one month. Echocardiography showed LV pseudoaneurysm and huge pericardial effusion. The pseudoaneurysm entrance was closed percutaneously. The third case was 3-months baby girl diagnosed with aortic coarctation (COA), patent ductus arteriosus (PDA), and muscular ventricular septal defect. She has repair of COA, pulmonary artery band (PAB), and PDA ligation at three weeks of age. Six weeks later developed sepsis. Echocardiography and CT revealed huge pseudoaneurysm at site of COA repair. Surgical resection of the huge pseudoaneurysm was done.
Conclusion: Meticulous evaluation and good utilization of the cardiac diagnostic tools will result in early diagnosis and management of the cardiac and vessel pseudoaneurysms which are usually fatal.
Keywords: Aortic coarctation, Endocarditis, Pseudoaneurysm
Introduction
Cardiac and great vessels pseudoaneurysm in pediatric patients is a rare complication of endocarditis, endarteritis, and post-cardiac surgery [1]. In endarteritis pseudoaneurysms occur as a complication of erosion of the inner layers of the arterial wall. The false aneurysm is covered by adventitia or adjacent tissues only [2]. Pseudoaneurysm can occur due to rupture of myocardium or vessel intima and restricted by adherent pericardium, adventitia, or scar tissue [3],[4]. It can lead to death if left untreated [4]. Post-cardiac surgery especially coarctation repair the sutures line may get infected, aggravated by the turbulence flow in situ.
Approach, modes of intervention and follow-up of cardiac and great vessels aneurysm in pediatric patients remain challenging. Surgical resection of ruptured tissue and closure of pseudoaneurysm is the main management options [5].
Percutaneous closure of the aneurysmal orifice is a challenging approach and less invasive; however, used in adult population [6].
Case Series
Case 1
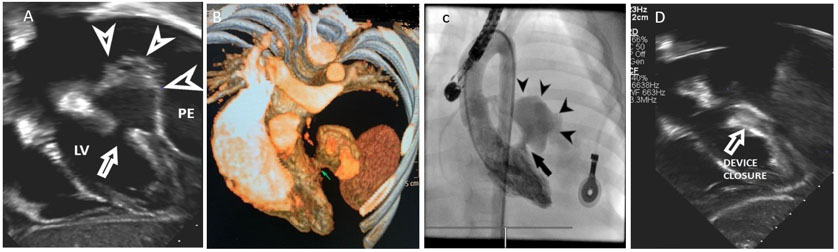
Twelve years old female admitted with headache, vomiting, and high-grade fever 39°C. She was pale, sick with tachypnea. Her pulse rate was 103/min, blood pressure 97/52 mmHg, and respiratory rate was 28/min. Chest X-ray showed cardiomegaly. Her laboratory tests revealed white blood cells count of 15×109/mm3 hemoglobin of 7.3 g/dL and high C-reactive protein of 222 mg/L. Blood culture revealed growth of methicillin resistant staphylococcus aureus (MRSA). The patient was diagnosed to have endocarditis. Echocardiography revealed multiple vegetations on the mitral valve leaflets and severe MV regurgitation. Massive pericardial effusion. Computed tomography (CT) scan of the brain showed cerebral abscesses. She was started on antibiotics. Further, during her hospital course she developed left-sided hemiparesis, her general condition deteriorated and the pericardial effusion increased thus a pericardial drain was inserted. Later, she was taken for a lifesaving cardiac surgery. Intraoperative, trans-esophageal echocardiography (TEE) showed pedunculated masses attached to anterior mitral leaflet (>2 cm in size) and anterior leaflet perforation (A2). There were ruptured chordae with anterior leaflet segment 3 (A3) prolapse (Figure 1).
She underwent vegetation removal and MV repair. Post-surgery TEE showed mild MV regurgitation.
Extubated after 48 hours, serial echocardiography showed impaired LV function and mild pericardial effusion. She continued on antibiotic for one month. The patient improved and was stable. One-month later developed hypotension and cardiogenic shock. An urgent transthoracic echocardiography showed huge pseudoaneurysm extending posterior to LV. The aneurysm orifice was in the LV lateral wall, inferior to the MV. There was pericardial effusion and mild MR (Figure 1B). She was taken for urgent surgery in the form of aneurysmectomy and patch repair of the ruptured LV lateral wall site.
Under conventional cardiopulmonary bypass, the clots were removed from the lateral and inferior surface of the LV, the huge pseudoaneurysm extended lateral and posterior to the LV was opened and found to be communicated to LV through two holes at the posterior lateral basal segment. The aneurysmal sac was resected and the hole in the LV lateral wall was patched using bovine pericardial patch and reinforced using polytetrafluoroethylene PTEE Polymer Pledgets. Postoperative echocardiography showed no leak at situ, mild mitral regurgitation, and good myocardial function.
The patient had antibiotic for six weeks and discharged in stable clinical condition. Eight months follow-up was satisfactory.
Case 2
Three and half years old previously healthy girl presented with high grade fever (39.5°C), abdominal pain, vomiting, and cough with shortness of breath. Chest X-ray showed clear lung field and cardiomegaly. Her initial blood tests showed evidence of infection, but no growth in her blood. She was commenced on intravenous immunoglobins, and antibiotics.
Her general condition did not improve and developed skin petechial and finger swellings. Her symptoms did not fit into criteria of specific systemic diseases. All laboratory investigations were unremarkable. Echocardiography showed pericardial effusion and LV posterior wall pseudoaneurysm. Cardiac tomography documented the findings (Figure 2).
After discussion with the team, it was decided to take her for percutaneous device closure of the aneurysmal orifice under guide of fluoroscopy and TEE using Amplatzer Muscular Occluder device size 12 mm through a retrograde approach (Figure 2). The procedure was uneventful.
In the following day, the echocardiography showed device in place closing the aneurysmal defect with no flow and mild pericardial effusion (Figure 2).
The patient improved dramatically after the procedure and kept on antibiotics for additional four weeks and heparin. At two-month follow-up was satisfactory.
Case 3
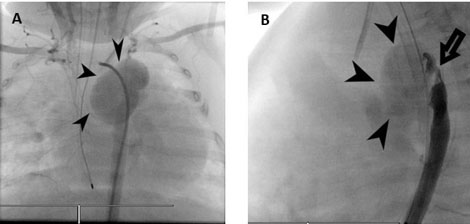
A three months old girl who was diagnosed with severe long segment COA, patent ductus arteriosus (PDA), and large mid muscular ventricular septal defect (VSD). At three weeks of age, she underwent coarctation repair with pericardial patch, PDA ligation, and pulmonary artery (PA) banding (Figure 3).
Postoperatively she was stable and echocardiogram revealed mild residual coarctation, PAB gradient 54 mmHg. Six weeks later the patient presented with respiratory distress and admitted to intensive care unit, she developed sepsis and cardiogenic shock which was not responding to supportive management. Blood cultures showed growth of Pseudomonas aeruginosa. A transthoracic echocardiography demonstrated a huge pseudoaneurysm close to the aortic arch patch (Figure 3).
Computed tomography revealed pseudoaneurysm at the surgical site distal to the origin of the left subclavian artery. There was fistulous connection to the left main pulmonary artery. The large pseudoaneurysm causes compression of the descending aorta distal to it.
After discussion among the treating group, she was taken for surgery. Intraoperatively they found a huge true aortic aneurysm extending from the left subclavian artery with a fistulous connection to the pulmonary artery at the site of PDA. The aneurysm was removed and the connection to main PA was closed using Gortex patch. The coarctation area was repaired by tube anastomosis from proximal arch to the descending aorta.
After surgery the patient was shifted to cardiac intensive care unit, monitored and stabilized. Echo postoperative showed no residual coarctation and no aneurysmal dilatation. The patient was discharged home after three weeks, her follow-up was satisfactory.
Discussion
The mycotic pseudoaneurysm is rare in children and fatal due to the risk of rupture [1].
All our three cases have endocarditis or endarteritis. All except one has documented bacterial growth, the one with negative blood culture received many antibiotics before its presentation, therefore may be partially treated infection.
In two cases the aneurysmal dilatation was treated surgically by resection and closure of the aneurysmal sac. However, in one case the treatment was through percutaneous closure of the aneurysmal orifice. The three patients improved in their cardiac status and returned well to their normal life.
In our first case the reason was endocarditis with methicillin resistant staph aureus, which has been reported earlier as a cause of endocarditis with development of LV aneurysm [7]. In addition, this patient underwent surgical MV repair which can be one of the factors for the development of pseudoaneurysm [4].
In the second case the endocarditis/myocarditis and aneurysm formation has developed in a patient with a normal heart which is free of any known systemic illness. Imaging revealed the aneurysmal defect to be suitable for device closure but needed to be implanted accurately so as not to affect the chordae of the MV. Additionally, with inflamed myocardium the LV wall perforation during catheter manipulation and device deployment should be put in consideration.
Percutaneous closure of aneurysm is a modality of treatment in adult population, but to date the only modality of treatment in pediatrics is surgery [6].
Development of hemiparesis can be due to endocarditis as in the first patient with vegetations in the MV, or due to a clot formation in the LV during disease process, and due to the presence of large aneurysm causing blood stagnation within the aneurysmal sac, clot formation, and thrombosis [1].
In the third case a pseudoaneurysm developed as a result of endarteritis following coarctation of the aorta repair. Pseudoaneurysm with endarteritis is known to be caused due to the turbulent flow at the narrow segment and infected suture lines [7].
The residual mild coarctation may be a factor in developing mycotic pseudoaneurysm. Extensive imaging detected it and patient could have succumbed with a missed diagnosis of infection.
Untreated pseudoaneurysm may cause rupture, thromboembolism, and compression of underlying structures [7]. In addition, left ventricular pseudoaneurysm can cause arrhythmias and low cardiac output. The goal of therapy is to address the pseudoaneurysm in appropriate time with minimum complications to save patient’s life. Younger patient with predisposing factors like valvular surgery has better prognosis [4].
Conclusion
High sense of suspicion of pseudoaneurysm is required. In addition to transthoracic echo, transesophageal echocardiography and CT scan are important in giving exact position and size of pseudoaneurysm. Surgical intervention is the usual approach; however, percutaneous approach has emerged with minimal risk.
REFERENCES
1.
Yeh TC, Liu CP, Tseng CJ, Can PR, Liou JC. Left ventricular pseudoaneurysm caused by infective endocarditis. Acta Cardiol Sin 2014;30(4):346–9.
[Pubmed]

2.
Arora K, Das RR, Tandon R, Goyal K, Panda SS. Pseudoaneurysm of left ventricle following Staphylococcal pericarditis in a child. APSP J Case Rep 2015;6(3):26.
[Pubmed]

3.
Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol 1998;32(3):557–61. [CrossRef]
[Pubmed]

4.
Sartipy U, Ivert T, Ugander M. Blood in, blood out: Left ventricular pseudoaneurysm following mitral valve endocarditis. Interact Cardiovasc Thorac Surg 2013;16(4):547–8. [CrossRef]
[Pubmed]

5.
Prifti E, Bonacchi M, Baboci A, et al. Surgical treatment of post-infarction left ventricular pseudoaneurysm: Case series highlighting various surgical strategies. Ann Med Surg (Lond) 2017;16:44–51. [CrossRef]
[Pubmed]

6.
Neeraj A, Kumar V, Bisht D, Kumar V. Percutaneous closure of a left ventricular pseudoaneurysm: Case report with review of cases. IHJ Cardiovascular Case Reports (CVCR) 2020;4(3):104–7. [CrossRef]

7.
Barth H, Moosdorf R, Bauer J, Schranz D, Akintürk H. Mycotic pseudoaneurysm of the aorta in children. Pediatr Cardiol 2000;21(3):263–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
I would like to thank all the doctors and technicians in King Fahd Medical City who helped in achieving these results for these patients.
Author ContributionsGhada Shiekheldin M Abdullah - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abdulrahman Almoukirish - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Tagaldin - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mashail Bin Obaidan - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
El-Segaier Milad - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Ghada Shiekheldin M Abdullah et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.