|
Case Report
Maxillary anterior teeth with extensive root resorption treated with multidisciplinary approach: A case report
1 Professor, Department of Endodontics, Iguaçu University, Nova Iguaçu, Rio de Janeiro, Brazil
2 Private Clinic, Niteroi, Rio de Janeiro, Brazil
3 Department of Pediatric Dentistry, School of Dentistry, Estacio de Sá University of Rio de Janeiro, Rio de Janeiro, Brazil
4 Department of Endodontics, Iguaçu University, Nova Iguaçu, Rio de Janeiro, Brazil
5 Professor, Department of Periodontics, Iguaçu University, Nova Iguaçu, Rio de Janeiro, Brazil
Address correspondence to:
Carlos Henrique Sardenberg Pereira
Department of Periodontics, Av. Abílio Augusto Távora, 2134, Nova Iguaçu – RJ 26260-045,
Brazil
Message to Corresponding Author
Article ID: 101373Z01TC2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
de Carvalho Coutinho TM, Campello CS, Abdelnur JP, Ronquete V, Pereira CHS, Marceliano-Alves MF. Maxillary anterior teeth with extensive root resorption treated with multidisciplinary approach: A case report. Int J Case Rep Images 2023;14(1):8–13.ABSTRACT
Invasive cervical resorption is a type of external resorption, which is generally located in the cervical region of the tooth. The resorptive process can be caused by physiological, pathological, hormonal, and trauma factors. The present study aimed to report a case of invasive cervical resorption in tooth 12 identified as an incidental finding, in which all available clinical resources were used, as well as a combined multidisciplinary treatment of endodontics, orthodontics, surgery, and prosthesis. At the initial consultation, the tooth presented with Heithersay’s class II resorption, undergoing endodontic treatment and traction for subsequent cavity sealing. After completion of orthodontics, an increase in the resorptive pocket was observed (Class III of Heithersay), which led to endodontic retreatment and subsequent surgical intervention to remove the granulation tissue and fill it with bioceramic material. The preparation of the coronal remnant and fabrication of a prosthetic restoration were performed, with the aim of shielding the endodontic cavity and functionally restoring the tooth. With the case presented, it was possible to conclude that incidental findings are part of the endodontist’s daily life, requiring a constant search both for early diagnosis and effective multidisciplinary treatment, which contributes to the restoration of aesthetics and function, contributing to the tooth longevity.
Keywords: Biomaterials, Incidental findings, Tooth resorption
Introduction
Tooth resorption is a progressive dentin loss that can be traumatic or infectious origin related. The literature is not conclusive regarding the etiological factor of tooth resorption; however, there are correlated factors: dental trauma, orthodontic movement or even infections of the endodontic and periodontal system, or idiopathic [1].
Orthodontically induced inflammatory root resorption (OIIRR) is a common phenomenon that can be triggered by an adverse effect of orthodontics; however, it usually ceases when the force is removed [1],[2],[3]. The force applied during orthodontic treatment induces inflammation and can be related as one of the etiological factors of root resorption. Thus, it is suggested that the applied force be in the range of 20–150 g tooth G1 for the desired tooth movement. This type of resorption may present as a radiolucent lateral defect or shortening of root length [2],[3].
Invasive cervical resorption (ICR) is an external resorption, located in the cervical region, and may extend to apex. Several etiological factors can be related, but in the idiopathic resorption no endodontic infection is present and is usually associated with trauma or bacteria that are present in the gingival sulcus which led to chronic inflammation [2]. This process induces bone and root resorption due to the interaction of RANK and RANK-L proteins with blast and clastic cells. The clastic cells release hydrogen ions and proteolytic enzymes after bonding with the mineralized surface, causing the environment to become acidic and lead to tissue mineral loss [2],[3]. At optimal levels, this process is paralyzed, reestablishing the pH of the medium, interrupting the process of mineral losses. If there is no interruption, the imbalance is maintained, culminating in further tissue damage [4].
Clinically, this type of resorption shows a pink area in the cervical region and may present with bleeding on probing and associated cavitation [4]. In most cases, there is a percussion test and pulp sensitivity test compatible with pulp and periradicular health. Radiographically, incipient resorptions are not visualized, but in an extensive lesion, it is possible to notice an irregular radiolucent area with the non-involvement of the internal canal walls. The limitation of early diagnosis is that the patient is asymptomatic [4]. For treatment of early invasive cervical resorption with no pulp involvement endodontic treatment is not an option and follow-up is recommended. When a root canal infection is present, endodontic treatment is indicated, being associated with the sealing of the remaining dental defect with a bioceramic material [1],[2],[3],[4].
Bioceramics have high mechanical properties, tissue compatibility and promise to solve possible clinical complications. Initially, Mineral Trioxide Aggregate (MTA) was used to seal the apical portion and later used to seal possible perforations and stimulate the formation of a mineralized barrier in immature teeth [5],[6],[7], as well as biocompatibility, antimicrobial activity, good adhesion to dentin walls [6],[7]. But one of its main advantages is to stimulate cell proliferation and multiplication, causing the recovery of damaged tissue [6]. However, the difficulties are handling and handling the material, the discoloration of the tooth, and the long setting time [7].
Another bioceramic material is Biodentine (Maur-des-Fossés Cedex, França), which is composed of: tricalcium silicate, sodium carbonate, zirconium oxide, and calcium chloride [7],[8] and due to its chemical composition, it resembles hydroxyapatite and stimulates a skeleton for regeneration and repair tissue [8],[9]. Due to its mechanical properties, when in contact with the dentinal constituents, it can generate a reactional dentin through the mineralization process that consequently forms a dense dentin bridge. Other cited properties are good adhesion capacity and non-contraction after the setting reaction, insolubility against oral fluids, saliva or blood, antibacterial action, and above all not being irritating to adjacent tissues [6],[7],[8],[9].
In view of the above, the aim of the present study was to report a clinical case of an incidental finding of invasive cervical resorption treated with Biodentine.
Case Report
An 11-year-old ASA I (American Society of Anesthesiologists type I) patient attended the Dental Clinic for a routine evaluation in January 2018. In this consultation, a physical and radiographic examination was performed, in which the periapical radiograph showed an incidental finding, characterized by a radiolucent image in the region of this—cervical of tooth 12. According to the patient's dental history, in September 2014 he underwent extraction and a mesio-tooth in this region; however, tooth 12 had not yet started its eruption process. In November 2015, element 12 began its eruption process within the normal range. The patient underwent annual periodic follow-up and nothing noteworthy was observed. However, in 2017 there was no annual consultation.
In the periodic consultation carried out in 2018, a process of dental resorption in tooth 12 was radiographically diagnosed.
Clinical procedures
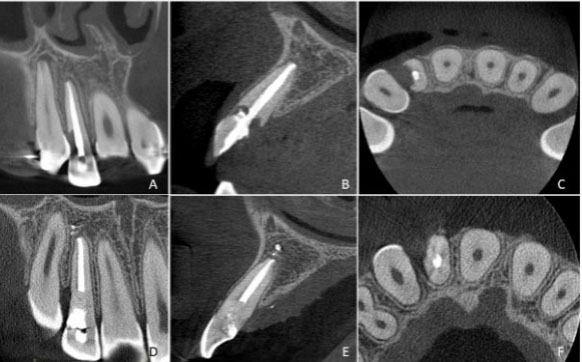
The radiographic examination showed an invasive cervical resorption (Figure 1A). Clinically, tooth 12 did not respond to cold pulp clinical tests, suggesting pulp necrosis. The patient underwent endodontic treatment in July 2018, which was performed with hybrid instrumentation, for the mechanized instrumentation the EASY ProDesign Logic #30/05 rotary system was used and for the completion of the apical stop a NITI # hand file 35. The intracanal medication used was the association of chlorhexidine and calcium hydroxide. The patient returned 20 days after the complete mechanical chemical preparation to complete the endodontic treatment. Invasive cervical resorption extended to the subgingival region, making it impossible to restore the defect.
Tooth 12 was submitted to orthodontic traction with the aim of enabling the restoration, this treatment option was initially considered with the aim of not causing a gingival margin defect and preventing the percolation of salivary fluids into the root canal system. After 10 months of follow-up after orthodontic traction, radiographically showed an increase in the resorptive lesion (Figure 1B) and therefore, a cone beam computed tomography (CBCT) was requested for a multiplanar evaluation of the lesion (Figure 2). Cone beam computed tomography showed severe invasive cervical resorption, which extended apically and communicated with the endodontic filling material. In February 2020, a surgical intervention was performed to remove all the granulation tissue in the region of resorption and subsequent filling with bioceramic material (Biodentine—Maur-des-Fossés Cedex, França) (Figure 1C).
Follow-up sessions were carried out periodically, 30 days, 3 months, 6 months, and 1 year, respectively, in which all consultations were recorded with digital periapical radiographic examination, which showed the bioceramic material adapted to the root surface; however, tooth 12 presented 5 mm periodontal pocket, bleeding, and suppuration in the distal region and the patient was referred for a periodontal evaluation.
In November 2021, it was decided to make a fiberglass post followed by a provisional poly(methyl methacrylate) (PMMA) crown milled in the computer aided design/computer aided manufacture (CAD/CAM) system in the remaining coronary, with the objective of better shielding the endodontic cavity and better periodontal control, thus enabling maintenance from the tooth until the moment of definitive prosthetic rehabilitation, since the patient has the desire to undergo orthodontic therapy for teeth alignment.
Because the resorption was large and wide, and there was a risk of root fracture, a customized glass fiber post was selected for the maxillary right lateral incisor due to the perforation and the fragility of the root. A direct technique was used to customize the post with resin composite to minimize the cementation line thickness as much as possible. The post and core were obtained using a radiolucent glass fiber post embedded in resin composite (Whitepost, FGM, Joinville, Brazil).
The root canal space preparations were made with a Largo bur (Dentsply–Maillefer), leaving approximately 5 mm of canal filling at the apex. The dowels were cemented with a self-adhesive resin-based cement (RelyX U200, 3M ESPE, St. Paul, MN), in accordance with the manufacturer’s directions. The core was prepared using a resin composite (Opallis, FGM, Joinville, Brazil) with smooth, slightly converging axial walls, well-defined margins, and 2 mm of incisal reduction. Next, we performed a full crown preparation and performed intraoral scanning, followed by design and milling in the CAD/CAM system (Omnicam and MCXl, Denstsply-Sirona, Germany) of the PMMa (Vita Cad Temp, Vita, Germany) crown (Figure 3).
Discussion
The exact etiology of invasive cervical resorption is still unclear and probably its cause has a multifactorial origin, with the maxillary incisors being the most affected teeth, this incidence was observed in one of the cases described. There is no predilection for age or sex, but there are several predisposing factors, among these factors stand out: trauma, orthodontic treatment, internal bleaching, and periodontal treatment that can cause physical damage to pre-cementum showing a strong relationship with invasive cervical resorption [10]. An anatomical defect between enamel and cementum at the cementoenamel junction, to which the underlying dentin is exposed, may also predispose to this condition. However, in the cases described above, there was no evident correlation of cause and effect with any of the etiological factors described in the literature, classifying invasive cervical resorption as idiopathic [2],[9],[10].
The highly vascularized resorptive granulomatous tissue that is found within the tooth makes it thinner and has irregular, translucent margins. The edges of the cavity are usually sharp and narrow, this causes it to usually change the color of the region to a pinkish spot, which is the main sign of clinical recognition of this pathology [4],[11]. In the present study, the cases described did not present changes in the color of the crown, which agrees with the descriptions by other study [4], who, although citing color changes as one of the main clinical signs, emphasizes that this clinical characteristic is not very prevalent in all cases, and may go unnoticed until periodontal and/or pulpal implications appear, through clinical and clinical examinations.
Routine radiographs
In most cases, invasive cervical resorption is asymptomatic and painless, exactly as can be observed in the present cases. However, in advanced cases symptoms, including pulp pain and tenderness, like symptoms of irreversible pulpitis or acute apical periodontitis may be seen [11],[12].
The main radiographic techniques used for diagnosis are the periapical intraoral technique and more recently, cone beam computed tomography. In cases of resorptions, the exact size and location of the lesion can be better quantified through CBCT, studies show that periapical radiography, as it is two-dimensional, is limited to perform an assessment of the size, circumferential propagation, and location of the lesion, when compared to a CBCT [2],[11],[12]. Due to the sensitivity of the CBCT method, it is recommended to use it as the main test for diagnosing and evaluating resorptive lesions.
The treatment of ICR depends on its severity and location, whether the defect has perforated the root canal system and the tooth’s restorative possibility [11],[12]. In cases of absence of pulp involvement, endodontic treatment should not be performed, and monitoring of this condition should be carried out [2],[3],[10]. The protocol in the current literature includes surgical access, total removal of resorptive tissue, topical application of 90% aqueous trichloroacetic solution, debridement, root canal treatment if the lesion has perforated the root canal, restoration of the resorptive defect by placing a filling material and follow-up examinations [11]. In the presented case, the treatment protocol followed the literature, presenting a previous stage that was the tooth orthodontic traction with the aim of reestablishing the biological space.
Additionally, a necessary surgical intervention was carried out, which allowed the access and the removal of the resorptive tissue and adequate defect filling, reducing the chances of recurrence [10],[11]. During the surgery, Emdogain (Straumann, Fontenay sous Bois, França) was used, which is made up of proteins derived from the enamel matrix, which, in addition to having antimicrobial properties, helps in periodontal regeneration [13],[14].
For the resorption defect sealing Biodentine was used. This cement is a calcium silicate based with a shorter time setting than MTA, with initial setting in 9 minutes and final setting in up to 45 minutes [7],[15]. Radiographic follow-up was performed periodically during the first year, which showed a union of the filling material with the tooth structure. This union is described in the literature as a push out union, being maintained even in contact with blood fluid and after irrigation with sodium hypochlorite or saline water [16],[17],[18].
The long-term success of the endodontic therapy is closely related to the success of the restorative procedure [17],[18]. In relation to the restoration of the tooth, the post space was too wide for using a single prefabricated post, glass fiber-reinforced post was used embedded in resin composite to diminish the amount of resin cement necessary. This issue is important because thick cement lines may negatively influence the bond strength of post cemented to the root dentin [19],[20],[21],[22]. The use of fiber-reinforced dowels associated with adhesive dentistry has increased the rate of success of such cases [19].
Conclusion
Dental findings are common within the dentist's routine and to solve certain cases, high quality materials are needed that optimize the time of the professional and the patient. Biodentine, in addition to being used in simpler cases, is also used to repair more complex cases so that the compromised element can have greater longevity in the oral cavity. The case report confirmed the control of tooth resorption, however, the follow-up of this element will be continued for the conclusion of the case.
REFERENCES
2.
Wahab RMA, Shafiai NAA, Ariffin SHZ. An insight into risk factors for root resorption during orthodontic treatment. J Med Sci 2017;17(1):1–9. [CrossRef]

3.
Ferreira MD, Barros-Costa M, Costa FF, Freitas DQ. The prevalence and characteristics of external cervical resorption based on cone-beam computed tomographic imaging: A cross-sectional study. Restor Dent Endod 2022;47(4):e39. [CrossRef]
[Pubmed]

4.
Galler KM, Brandl FP, Kirchhof S, et al. Suitability of different natural and synthetic biomaterials for dental pulp tissue engineering. Tissue Eng Part A 2018;24(3–4):234–44. [CrossRef]
[Pubmed]

5.
6.
Mona M, Abbasi Z, Kobeissy F, Chahbandar A, Pileggi R. A bioinformatics systems biology analysis of the current oral proteomic biomarkers and implications for diagnosis and treatment of external root resorption. Int J Mol Sci 2021;22(6):3181. [CrossRef]
[Pubmed]

7.
Raghavendra SS, Jadhav GR, Gathani KM, Kotadia P. Bioceramics in endodontics – A review. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S128–37. [CrossRef]
[Pubmed]

8.
Al-Haddad A, Che Ab Aziz ZA. Bioceramic-based root canal sealers: A review. Int J Biomater 2016;2016:9753210. [CrossRef]
[Pubmed]

9.
Jitaru S, Hodisan I, Timis L, Lucian A, Bud M. The use of bioceramics in endodontics – Literature review. Clujul Med 2016;89(4):470–3. [CrossRef]
[Pubmed]

10.
Malkondu Ö, Karapinar Kazandağ M, Kazazoğlu E. A review on biodentine, a contemporary dentine replacement and repair material. Biomed Res Int 2014;2014:160951. [CrossRef]
[Pubmed]

11.
Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus biodentine: Review of literature with a comparative analysis. J Clin Diagn Res 2017;11(8):ZG01–5. [CrossRef]
[Pubmed]

12.
Rotondi O, Waldon P, Kim SG. The disease process, diagnosis and treatment of invasive cervical resorption: A review. Dent J (Basel) 2020;8(3):64. [CrossRef]
[Pubmed]

13.
Tsaousoglou P, Markou E, Efthimiades N, Vouros I. Characteristics and treatment of invasive cervical resorption in vital teeth. A narrative review and a report of two cases. Br Dent J 2017;222(6):423–8. [CrossRef]
[Pubmed]

14.
Asgary S, Nourzadeh M, Verma P, Hicks ML, Nosrat A. Vital pulp therapy as a conservative approach for management of invasive cervical root resorption: A case series. J Endod 2019;45(9):1161–7. [CrossRef]
[Pubmed]

15.
Heithersay GS. Invasive cervical resorption following trauma. Aust Endod J 1999;25(2):79–85. [CrossRef]
[Pubmed]

16.
Wang HH, Sarmast ND, Shadmehr E, Angelov N, Shabahang S, Torabinejad M. Application of enamel matrix derivative (Emdogain) in endodontic therapy: A comprehensive literature review. J Endod 2018;44(7):1066–79. [CrossRef]
[Pubmed]

17.
Gión-Guerra B, Pérez-Lanza P, Almiñana-Pastor P, Micó-Martínez P, Alpiste-Illueca FM, López-Roldán A. Performance of the dentogingival junction with mta and biodentine on the treatment of invasive cervical resorptions. A literature review and case report. J Clin Exp Dent. 2021;13(1):e95–8. [CrossRef]
[Pubmed]

18.
de Carvalho MA, Lazari PC, Gresnigt M, Del Bel Cury AA, Magne P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz Oral Res 2018;32(suppl 1):e74. [CrossRef]
[Pubmed]

19.
Stenhagen S, Skeie H, Bårdsen A, Laegreid T. Influence of the coronal restoration on the outcome of endodontically treated teeth. Acta Odontol Scand 2020;78(2):81–6. [CrossRef]
[Pubmed]

20.
Ferrari M, Ferrari Cagidiaco E, Pontoriero DIK, Ercoli C, Chochlidakis K. Survival rates of endodontically treated posterior teeth restored with all-ceramic partial-coverage crowns: When systematic review fails. Int J Environ Res Public Health 2022;19(4):1971. [CrossRef]
[Pubmed]

21.
Saker S, Özcan M. Retentive strength of fiber-reinforced composite posts with composite resin cores: Effect of remaining coronal structure and root canal dentin conditioning protocols. J Prosthet Dent 2015;114(6):856–61. [CrossRef]
[Pubmed]

22.
Lazari PC, de Carvalho MA, Del Bel Cury AA, Magne P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J Prosthet Dent 2018;119(5):769–76. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Thais Machado de Carvalho Coutinho - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Carollyne Souza Campello - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Juliana Pires Abdelnur - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Vivian Ronquete - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Carlos Henrique Sardenberg Pereira - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marilia F Marceliano-Alves - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Thais Machado de Carvalho Coutinho et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.