|
Clinical Image
An unusual case of a retroperitoneal cyst in a child
1 King’s College Hospital, Denmark Hill, London SE5 9RS, United Kingdom
Address correspondence to:
Nigel Heaton
King’s College Hospital, Denmark Hill, London SE5 9RS,
United Kingdom
Message to Corresponding Author
Article ID: 101372Z01NG2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Grayson N, Younis M, Heaton N. An unusual case of a retroperitoneal cyst in a child. Int J Case Rep Images 2023;14(1):4–7.ABSTRACT
No Abstract
Keywords: Abdominal pain, Hemorrhagic cyst, Retroperitoneal cyst
Case Report
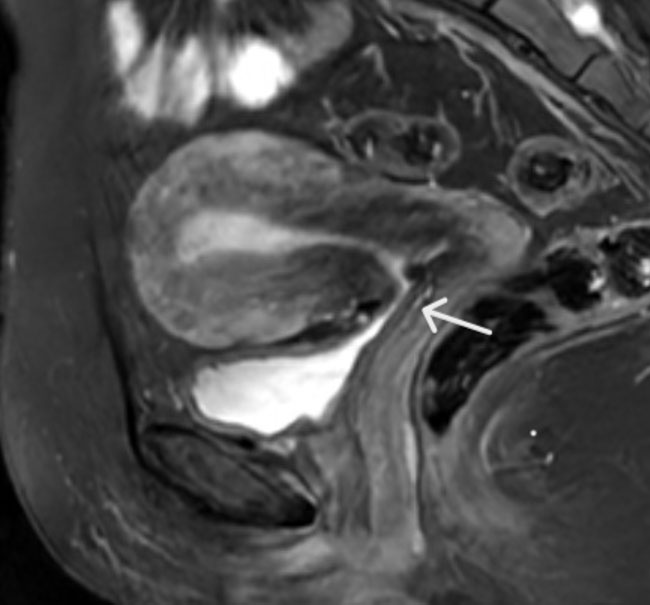
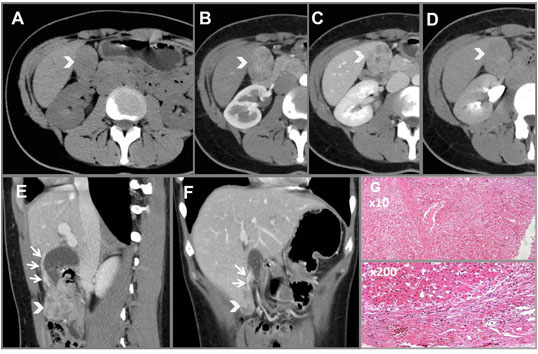
A previously well 9-year-old boy presented with intermittent left upper quadrant pain, anorexia, and weight loss over six months. His past medical history was significant for being born preterm at 34 weeks’ gestation and requiring ventilatory support as a neonate. Computed tomography (CT) scan (Figure 1 and Figure 2) showed a 10 cm encapsulated spherical mass appearing to arise from the pancreatic tail. The working diagnosis was a cystic pancreatic tumour, and he was referred for further management.
At subsequent laparotomy a retroperitoneal mass was found adherent to the left colon and duodenum but free from the pancreas, with associated reactive lymphadenopathy. The mass was biopsied, and surgery was abandoned to allow for formal histological evaluation. Frozen section histology reported a spindle cell lesion comprising of bland spindle cells with elongated cigar-shaped nuclei. Necrosis was present at one end of the core biopsy. Mitotic activity was not seen. Immunohistostaining showed spindle cells expressing smooth muscle actin, desmin, and vimentin. There was no significant expression of S100, CD117, CD34, or AE1/AE3. There was no nuclear or cytoplasmic beta catenin expression. Up to three IgG4 expressing plasma cells were seen per high power field.
Further work-up included a computed tomography positive emission tomography (CT PET) scan which showed a non-avid mass appearing to arise from the tail of the pancreas. Computed tomography-guided biopsy showed degenerate and viable red cells. No other cell type was identified to help determine the nature of the lesion. A decision was made to perform local resection as no malignancy was identified. At surgery the lesion was excised locally without compromising adjacent pancreas, colon, or small bowel. He recovered well post-operatively and was discharged home on day 4. Final histology showed a 130 mm encapsulated thick-walled organized hematoma with no evidence of malignancy.
Discussion
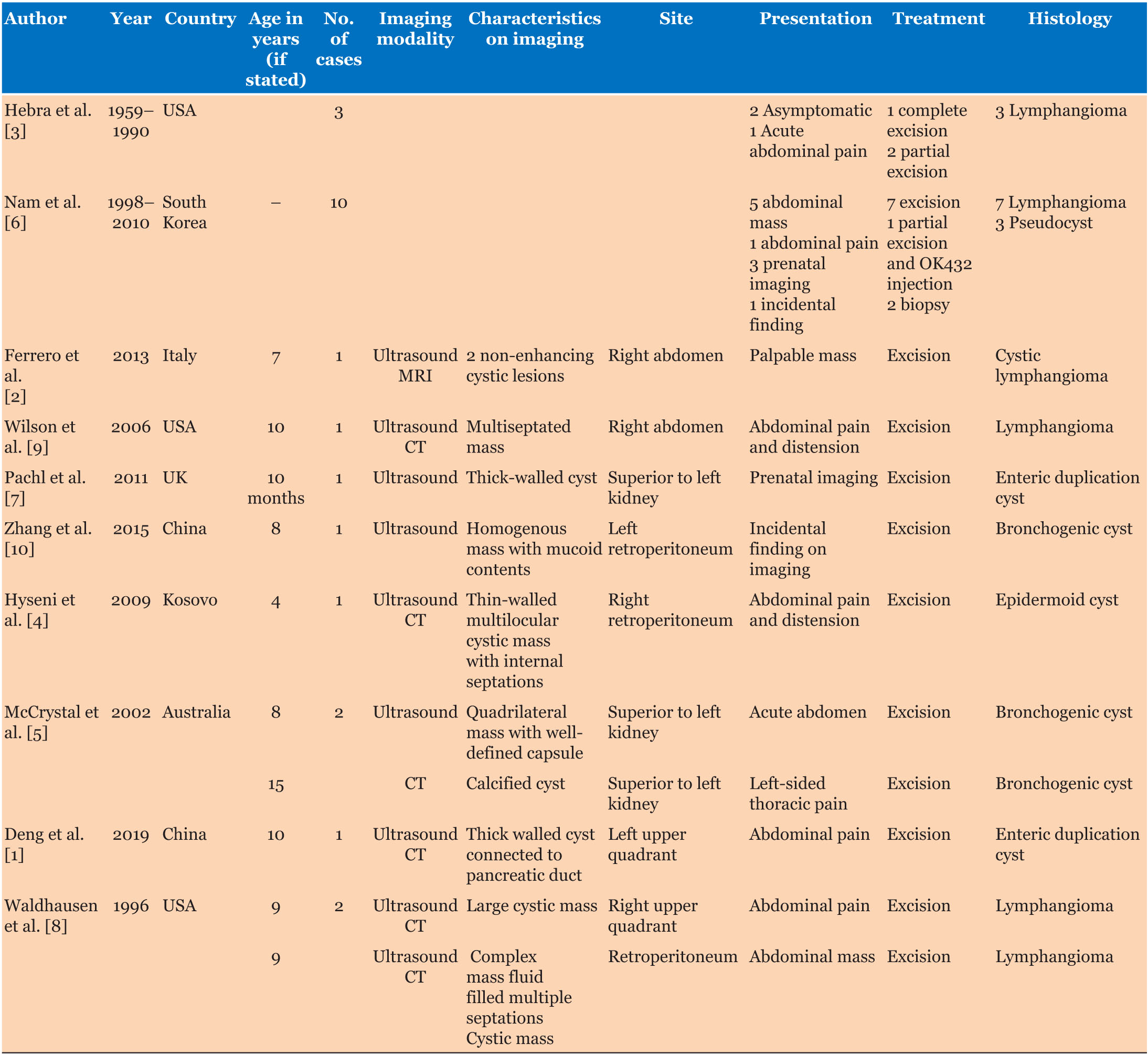
Retroperitoneal cysts are rare with few reports in children. A literature review of PubMed was performed using the search terms retroperitoneal cyst in children and pediatric population. Articles not available in English, pancreatic cysts and patients over age 18 were excluded. The results are summarized in Table 1 [1],[2],[3],[4],[5],[6],[7],[8],[9],[10].
The presenting symptoms are non-specific and varied with abdominal pain and distension being the most common. Other presentations included nausea and vomiting, anorexia, acute abdomen, and incidental detection on examination or on imaging.
The differential diagnosis includes cysts of lymphatic origin and lymphangiomas, benign or malignant mesothelial cysts, enteric cysts, cysts arising from a urogenital origin, dermoid cysts and cysts with traumatic, hemorrhagic or infectious etiology [1].
The reported ages of patients varied from 10 months old to 15 years old with a median age of 9 years old for those included.
Investigations varied from case to case. Ultrasound was the most commonly used modality across all of the patients.
Diagnosis can be difficult. The literature review confirmed that the majority of cases were diagnosed as retroperitoneal cysts at operation. On imaging, the cyst appeared to be associated with the tail of the pancreas but at operation, it was clearly separate and in our case, there was concern that it could malignant. Frozen section revealed spindle cells within the wall and it required formal immunohistostaining and repeat biopsy to exclude malignancy.
Retroperitoneal cysts are treated surgically. Acutely there is a risk of cyst rupture, infection, and hemorrhage. They may cause abdominal pain by compression of surrounding organs [1]. In this case, complete excision was achieved without complication.
Conclusion
- Retroperitoneal cysts are a rare entity with a wide diagnosis. Here we report a non-traumatic hemorrhagic cyst which has not been reported previously and should be included in the differential diagnosis.
- The presenting symptoms of retroperitoneal cysts vary widely from patient to patient in this literature review.
- This patient underwent a long diagnostic process which we hope to avoid with documentation of this case.
REFERENCES
1.
Deng Y, Hu Z, Liao J, Hao W, Hu G. Isolated retroperitoneal enteric duplication cyst associated with an accessory pancreatic lobe. Int J Clin Exp Pathol 2019;12(8):3089–95.
[Pubmed]

2.
Ferrero L, Guanà R, Carbonaro G, et al. Cystic intra-abdominal masses in children. Pediatr Rep 2017;9(3):7284. [CrossRef]
[Pubmed]

3.
Hebra A, Brown MF, McGeehin KM, Ross AJ 3rd. Mesenteric, omental, and retroperitoneal cysts in children: A clinical study of 22 cases. South Med J 1993;86(2):173–6. [CrossRef]
[Pubmed]

4.
Hyseni NS, Llullaku SS, Koçinaj DH, Jashari HJ, Kelmendi BZ. An unusual location of retroperitoneal epidermoid cyst in a child: Case report and a review of the literature. Cases J 2009;2:9397. [CrossRef]
[Pubmed]

5.
McCrystal DJ, Borzi PAJ. Retroperitoneoscopic resection of retroperitoneal bronchogenic cysts. Pediatr Surg Int 2002;18(5–6):375–7. [CrossRef]
[Pubmed]

6.
Nam SH, Kim DY, Kim SC, Kim IK. The surgical experience for retroperitoneal, mesenteric and omental cyst in children. J Korean Surg Soc 2012;83(2):102–6. [CrossRef]
[Pubmed]

7.
Pachl M, Patel K, Bowen C, Parikh D. Retroperitoneal gastric duplication cyst: A case report and literature review. Pediatr Surg Int 2012;28(1):103–5. [CrossRef]
[Pubmed]

8.
Waldhausen JH, Holterman MJ, Tapper D. Identification and surgical management of cystic retroperitoneal lymphangioma in children. Pediatr Surg Int 1996;11(4):283–5. [CrossRef]
[Pubmed]

9.
Wilson SR, Bohrer S, Losada R, Price AP. Retroperitoneal lymphangioma: An unusual location and presentation. J Pediatr Surg 2006;41(3):603–5. [CrossRef]
[Pubmed]

10.
Zhang D, Zhang Y, Liu X, et al. Challenge in preoperative diagnosis of retroperitoneal mucinous cyst in a pediatric patient. Int J Clin Exp Med 2015;8(10):19540–7.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Niamh Grayson - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Muhammad Younis - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nigel Heaton - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Niamh Grayson et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.