|
Case Report
Calcifying odontogenic cyst causing an atypical complication: Case report
1 Dentistry Department, University of Taubate, Taubaté, SP, Brazil
2 Private Oral and Maxillofacial Surgery Service, São Paulo, SP, Brazil
3 Dentistry Department, University Center of Braz Cubas, Mogi das Cruzes, SP, Brazil
4 Dentistry Department, University Educational Society of Santa Catarina, Joinville, SC, Brazil
5 Private Service, CK Estomatologia, São Paulo, SP, Brazil
Address correspondence to:
Thayná Melo de Lima Morais
Ph.D, Private Service, CK Estomatologia, Rua Catulo da paixão cearense, Vila Saúde, São Paulo, SP, Postal code: 04145-010,
Brazil
Message to Corresponding Author
Article ID: 101368Z01AB2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Barreto ALA, Utumi ER, Kitakawa D, da Silva Peralta F, de Lima Morais TM, de Carvalho LFCS. Calcifying odontogenic cyst causing an atypical complication: Case report. Int J Case Rep Images 2022;13(2):233–236.ABSTRACT
Introduction: Calcifying odontogenic cyst (COC) is a benign cystic type of odontogenic tumor, without neoplastic character and unusual in nature. Its development is slow and asymptomatic, being characterized by a mass that affects the maxilla and mandible.
Case Report: A 40-year-old male presented with mild extra and intraoral facial swelling in the region of the right upper incisors, without symptoms. On intraoral examination, he observed intact and normal colored buccal mucosa. Radiographic examination showed a radiolucent lesion between teeth 11 and 12. Excisional biopsy was performed. The histological diagnosis was calcifying odontogenic cyst.
Conclusion: Calcifying cyst is an uncommon odontogenic cyst that most often occurs in the maxilla. However, it should be in the differential diagnosis of other odontogenic lesions. In addition, after conservative surgical removal, long-term follow-up is recommended. Because, although rare, recurrence can occur.
Keywords: Calcifying odontogenic cyst, Gorlin cyst, Jaw cyst
Introduction
Calcifying odontogenic cyst (COC) is the new term suggested in 2017 by the World Health Organization (WHO) to replace the designation calcifying cystic odontogenic tumor, thus referring to the benign cystic type of odontogenic tumor, without neoplastic character [1],[2],[3].
Calcifying odontogenic cyst is an uncommon lesion originating from the odontogenic epithelium, of unknown pathogenesis, being rare when formed by abnormally keratinized ghost cells, which can undergo calcifications [4],[5].
The classic cases are asymptomatic, affecting the maxilla or mandible of young patients of both the sexes, with an average age of 30 years, showing slow growth and local swelling [4],[6].
Some lesions have more solid characteristics, others more cystic, with great radiographic variation. Sometimes presenting as a well-circumscribed, unilocular radiolucent lesion with irregular radiopaque areas in its interior, sometimes as spherical calcifications with indistinct spots [7],[8].
Histologically, COC is composed of layers and nests of polyhedral and eosinophilic epithelial cells, which may also present cellular abnormalities, giant cell formation, and nuclear pleomorphism [9]. The classic characteristic of COC is the findings of amorphous, sometimes hyalinized, eosinophilic extracellular material, which presents positive staining for amyloid and calcifications present in various ways [10].
Biopsy is indicated for diagnosis and complementary imaging exams are important for surgical planning, which consists of enucleation of the lesion followed by curettage [2],[10].
As it is infrequent and of unknown pathogenesis, the COC case reports contribute to new information about the behavior and the lesion, reaffirming the removal techniques. Thus, this paper reports a case in which the development of COC in the central incisor region caused tooth root divergence and root resorption.
Case Report
Male patient, 40 years old, white, with type 2 diabetes mellitus, hypertensive, overweight, and non-smoker, presented mild extra and intraoral facial swelling in the region of the upper right incisors and was referred by a dentist to the clinic specializing in dentistry for assessment.
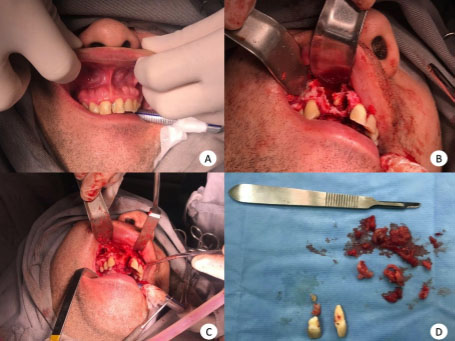
The patient was asymptomatic and the intraoral examination showed, in addition to swelling, maxillary exostosis, mucosa with normal appearance and tooth mobility 11 (Figure 1).
The panoramic radiograph showed a radiolucent lesion in the apical region of the right incisors, being particularly delimited between the middle third and apex of tooth 11 and with external root resorption of tooth 12 (Figure 2).
Incisional biopsy revealed COC and the proposed treatment was surgical removal in a hospital environment, under general anesthesia, with excisional biopsy and osteotomy (Figure 1).
During the extraction of teeth 11 and 12, it was noted that the cyst caused the root rupture of the central incisor separating the middle third from the apical third. The postoperative period was within the parameters and the patient is still recovering for the rehabilitation process.
Discussion
Calcifying odontogenic cyst was first described as a distinct clinicopathological entity by Gorlin and his colleagues in 1962. As it is an uncommon lesion with a diversity of characteristics and manifestations, there is some confusion regarding terminology. Thus, the lesion is also known as Gorlin’s cyst, calcifying odontogenic cyst and ghost cell odontogenic tumor [4],[11].
In 2017, WHO defined the term COC to designate this benign lesion, of cystic character, containing a variable number of ghost cells that can suffer calcifications [2],[11],[12] The term dentinogenic phantom cell tumor (TDCF) is the one suggested for the solid benign version containing ghost cells; and calcifying odontogenic tumor designed only for neoplastic lesions [3],[12].
It is known that COC is an uncommon lesion, with low prevalence among all odontogenic cysts, non-neoplastic, slow growing, and asymptomatic, affecting patients between 30 and 40 years old in the maxilla or mandible region, with no gender predilection and no reports of relapse. Differential diagnosis is made by histopathological examinations and aims to distinguish the lesion from common gingival fibroids, gingival cysts, adenomatoid odontogenic tumor, and peripheral giant cell lesion [4],[8],[13],[14].
Histologically, COC has a fibrous cystic wall, lined with odontogenic epithelium and containing cuboid or columnar basal cells. There may also be tissue that looks similar to the stellate reticulum of the enamel organ. Ghost cells, on the other hand, are evidenced by the presence of large, circular, anucleated and eosinophilic cells, which can be calcified with the presence of dysplastic dentin, usually located close to the basal layer of the epithelium. The lesions have in common the abnormal keratinization of odontogenic epithelial cells. Such presence of odontogenic cytokeratin may be involved in its development, since COC3 is derived from remnants of the odontogenic epithelium that remains within the jaws or gums [11],[14],[15].
The radiography of the lesion often presents an unilocular radiolucent area with well-defined margins [12], and irregular radiopaque areas within the lesion, or calcifications with indistinct spots [8].
Most cases cause changes in adjacent teeth, such as root resorption, displacement, divergence, and tooth impaction. Tooth divergence and root resorption can easily be found on conventional radiographs, but computed tomography can reveal more lesion details, such as the occurrence of tooth impaction, local expansion, and the presence of radiopaque peripheric bodies [15],[16]. Dental impaction or displacement in posterior of mandible, and the absence of these findings for lesions positioned anteriorly may be indicative of the moment of development of COC [8].
Diabetes mellitus and hypertension are systemic conditions that affect the oral cavity, favor the emergence of pathologies, and hinder the ability to recover and heal. Patients with such morbidities have higher rates of need for tooth extraction in cases of trauma and infections, as well as requiring different treatment goals and definitions of success from a healthy patient [17]. However, there are no studies that correlate the manifestation of COC in diabetic patients.
Conventional treatment is total enucleation of the cyst followed by curettage [4]. It is also recommended to remove 1–2 mm of bone layer around the lesion, removing the epithelial remains to avoid recurrences [17]. The absence of recurrence can be attested by radiographic control [12].
Despite being an uncommon lesion, the calcifying odontogenic cyst has very similar conditions when it manifests itself, whether due to its clinical aspects or to alterations in the teeth adjacent to the affected region.
Its removal in a hospital environment is highly recommended, as well as planning preceded by radiographs and incisional biopsies.
There are no studies that correlate diabetes mellitus with the occurrence of COC, and the patient’s systemic condition did not interfere in the intraoperative period or in his recovery.
Conclusion
Calcifying cyst is an uncommon odontogenic cyst that most often occurs in the maxilla. However, it should be in the differential diagnosis of other odontogenic lesions. In addition, after conservative surgical removal, long-term follow-up is recommended. Because, although rare, recurrence can occur.
REFERENCES
1.
de Arruda JAA, Monteiro JLGC, Abreu LG, et al. Calcifying odontogenic cyst, dentinogenic ghost cell tumor, and ghost cell odontogenic carcinoma: A systematic review. J Oral Pathol Med 2018;47(8):721–30. [CrossRef]
[Pubmed]

2.
Utumi ER, Pedron IG, da Silva LP, Machado GG, Rocha AC. Different manifestations of calcifying cystic odontogenic tumor. Einstein (Sao Paulo) 2012;10(3):366–70. [CrossRef]
[Pubmed]

3.
Irani S, Foroughi F. Histologic variants of calcifying odontogenic cyst: A study of 52 cases. J Contemp Dent Pract 2017;18(8):688–94. [CrossRef]
[Pubmed]

4.
5.
Yukimori A, Oikawa Y, Morita KI, et al. Genetic basis of calcifying cystic odontogenic tumors. PLos One 2017;12(6):e0180224. [CrossRef]
[Pubmed]

6.
Manohar B, Baidya D, Shetty N, Mathur A, Makhijani B. Calcifying epithelial odontogenic cyst. J Exp Ther Oncol 2017;12(2):151–6.
[Pubmed]

7.
Iida S, Fukuda Y, Ueda T, Aikawa T, Arizpe JE, Okura M. Calcifying odontogenic cyst: Radiologic findings in 11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101(3):356–62. [CrossRef]
[Pubmed]

8.
Moreno-Rodríguez P, Guerrero LM, Gómez-Delgado A, Castro-Núñez J. Active decompression and distraction sugosteogenesis for the treatment of calcifying odontogenic cyst. Oral Maxillofac Surg 2020;25(1):89–97. [CrossRef]
[Pubmed]

9.
Philipsen HP, Reichart PA. Calcifying epithelial odontogenic tumour: Biological profile based on 181 cases from the literature. Oral Oncol 2000;36(1):17–26. [CrossRef]
[Pubmed]

10.
Channappa NK, Krishnapillai R, Rao JBM. Cystic variant of calcifying epithelial odontogenic tumor. J Investig Clin Dent 2012;3(2):152–6. [CrossRef]
[Pubmed]

11.
Moleri AB, Moreira LC, Carvalho JJ. Comparative morphology of 7 new cases of calcifying odontogenic cysts. J Oral Maxillofac Surg 2002;60(6):689–96. [CrossRef]
[Pubmed]

12.
13.
Arruda JA, Silva LV, Silva L, et al. Calcifying odontogenic cyst: A 26-year retrospective clinicopathological analysis and immunohistochemical study. J Clin Exp Dent 2018;10(6):e542–7. [CrossRef]
[Pubmed]

14.
Fregnani ER, Pires FR, Quezada RD, Shih IM, Vargas PA, De Almeida OP. Calcifying odontogenic cyst: Clinicopathological features and immunohistochemical profile of 10 cases. J Oral Pathol Med 2003;32(3):163–70. [CrossRef]
[Pubmed]

15.
16.
Uchiyama Y, Akiyama H, Murakami S, et al. Calcifying cystic odontogenic tumour: CT imaging. Br J Radiol 2012;85(1013):548–54. [CrossRef]
[Pubmed]

17.
Mauri-Obradors E, Estrugo-Devesa A, Jané-Salas E, Viñas M, López-López J. Oral manifestations of diabetes mellitus. A systematic review. Med Oral Patol Oral Cir Bucal 2017;22(5):e586–94. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Anna Laura Almeida Barreto - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Estevam Rubens Utumi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dárcio Kitakawa - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Felipe da Silva Peralta - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Thayná Melo de Lima Morais - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Luis Felipe das Chagas e Silva de Carvalho - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Anna Laura Almeida Barreto et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.