|
Case Report
Miliary mottling and pleural metastases secondary to lung adenocarcinoma: A case report
1 Kingman Regional Medical Center, Kingman, Arizona 86409, USA
Address correspondence to:
Waheed Abdul
Kingman Regional Medical Center, Kingman, Arizona 86409,
USA
Message to Corresponding Author
Article ID: 101303Z01WA2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Abdul W. Miliary mottling and pleural metastases secondary to lung adenocarcinoma: A case report. Int J Case Rep Images 2022;13:101303Z01WA2022.ABSTRACT
Miliary mottling/metastases are defined as distinctive numerous small nodules (<3 mm) with sharp margins scattered throughout the lungs which can be seen on chest radiograph that are rarely associated with lung adenocarcinomas. We present a rare case of a 67-year-old smoker diagnosed with lung adenocarcinoma with metastatic pleural effusion and miliary mottling which highlights this rare association. Lung adenocarcinoma with miliary metastases have higher mortality rate and are associated with +ve epidermal growth factor receptor (EGFR) mutations.
Keywords: Lung adenocarcinoma, Miliary metastases, Miliary mottling, Pleural metastases
Introduction
Miliary mottling/metastases are defined as distinctive numerous small nodules (<3 mm) with sharp margins scattered throughout the lungs which can be seen on chest radiograph [1],[2]. The most common cause of miliary metastases is from tuberculosis, sarcoidosis, histoplasmosis, and occupational lung disease such as pneumoconiosis [1]. Other causes of miliary mottling are due to the secondary metastases from thyroid carcinoma, melanoma, osteosarcoma, renal cell carcinoma, testicular tumors, colorectal carcinoma, and very rarely from lung malignancy [1],[2].
Lung cancer is classified into small cell lung cancer and non-small cell lung cancer (NSCLC) and is one of the leading causes of death in the world [2]. Non-small cell lung cancer is subdivided into squamous cell carcinoma, large cell carcinoma, and adenocarcinoma.
Lung adenocarcinoma usually presents as ground-glass solid nodules and/or pleural effusion on radiography but it rarely presents with miliary metastases [1]. We present a rare case of lung adenocarcinoma with metastatic pleural effusion and miliary mottling.
Case Report
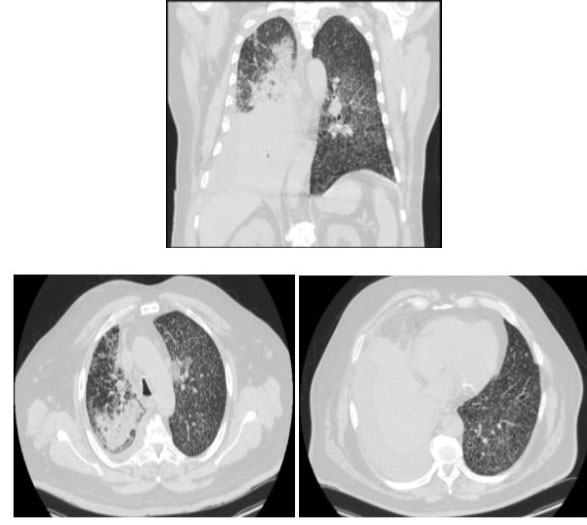
A 67-year-old male with current smoking history of 50 pack years was admitted for three days of persistent productive cough associated with dyspnea on exertion. On review of system, the patient had more than 30 lb weight loss in past six months. In the emergency room (ER), the patient was found to be hypoxic requiring 3 L nasal cannula (NC) oxygen but otherwise hemodynamically stable. His COVID test was negative. However, his chest radiograph showed extensive miliary opacities throughout both lungs with large right pleural effusion and upper mediastinum lymphadenopathy (Figure 1). The patient was placed on airborne precautions to rule out tuberculosis (TB). His acid-fast bacteria (AFB) stains, sputum culture, coccidioidomycosis panel, and TB quantiferon were negative. The patient underwent right-sided thoracentesis with placement of pleural drain. His pleural effusion work-up showed exudative process (Table 1). A computed tomography (CT) chest was performed which was significant again for severe diffuse miliary metastases and dense consolidation in the right middle/lower lobes consistent with pleural effusion (Figure 2). The dense consolidation and the exudative pleural effusion indicated very suspicious for lung cancer. The pleural effusion pathology was positive for primary moderately differentiated lung adenocarcinoma with positive CK7, CK20, and thyroid transcription factor (TTF) markers.
Oncology was consulted. A tissue biopsy was obtained which showed epidermal growth factor receptor (EGFR) positive with exon 19 deletion. Based on the clinical, imaging, and pathological findings, the patient was diagnosed with stage 4 lung adenocarcinoma with pleural and miliary metastases. The patient was discharged with 3 L NC oxygen with referral to our local oncology center.
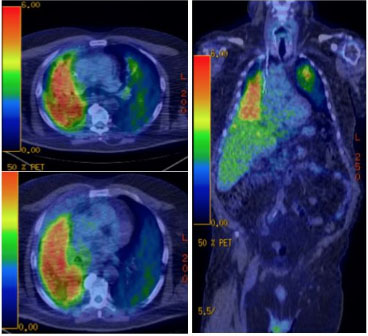
As outpatient, the patient had a positron emission tomography (PET) scan, magnetic resonance imaging (MRI) brain, and 2D echo as per recommendations of our oncology center. His PET scan showed hypermetabolic right pleural effusion and hilar mediastinal lymph nodes with hypermetabolic dense consolidative opacities in the right lower lobe with scattered hypermetabolic tree-in-bud and ground-glass opacities throughout both lungs (Figure 3).
His 2D echo showed normal ejection fraction and his MRI brain did not show any metastases. He was subsequently started on Alimta/Carboplatin/Pembrolizumab chemotherapy with addition of Osimertinib for EGRF positive mutation. Currently, the patient is continuing to follow-up with our local oncology center.
Discussion
Lung adenocarcinoma is the most common primary lung cancer—approximately 50% of all of the cases [2]. They usually arise in peripheral location of the lungs with pleural involvement. It demonstrates an acinar, papillary, micropapillary, lepidic, or solid growth pattern. Lung adenocarcinoma consists of abnormal glandular epithelium with degrees of architecture and differentiation of these glands.
In rare cases, lung adenocarcinoma can present with miliary metastases that are scattered throughout the lungs bilaterally as evident from our literature search [2]. Based on a PubMed search, there are only a handful of reports of such cases. Also, there are no large studies or population date of lung adenocarcinoma with miliary metastases up to date.
Lung adenocarcinoma with positive EGFR mutation (exon 19 deletion or exon 21 point addition) can be associated with miliary metastases [3]. Hsu et al. showed that patients with +ve EGFR mutations are three times more likely to have miliary metastases [4]. In our case, our patient had +ve EGFR mutation with exon 19 deletion. Albeit, cases with miliary metastases and +ve EGFR mutation carry shorter survival rate but they do respond to tyrosine kinase inhibitor (TKI) [5]. Our patient was placed on Osimertinib, which is a TKI in addition to standard chemotherapy [6].
Our case is more rare due to the presence of metastatic pleural effusion in addition to the miliary mottling. There are no published case reports in the literature that describes both phenomena arising from lung adenocarcinoma. However, the standard of care is the same for all metastatic lung adenocarcinomas.
Conclusion
In conclusion, our case report highlights a rare association of lung adenocarcinoma with miliary and pleural metastases with the clinical importance of ruling out all other differential diagnosis (tuberculosis, sarcoidosis, histoplasmosis, occupational lung disease, and other malignancies). Lung adenocarcinoma with miliary metastases have higher mortality rate and are associated with +ve EGFR mutations.
REFERENCES
1.
Pillai S, Khan A, Khan S. Adenocarcinoma of the lung presenting with intrapulmonary miliary metastasis. Cureus 2019;11(8):e5430. [CrossRef]
[Pubmed]

2.
Khan D, Danjuma M, Saddique MU, Murshed KAH, Yassin MA. Adenocarcinoma of the lung mimicking miliary tuberculosis. Case Rep Oncol 2020;13(1):139–44. [CrossRef]
[Pubmed]

3.
Schaller A, Beau-Faller M, Mennecier B, et al. Lung adenocarcinoma with pulmonary miliary metastases and complex somatic heterozygous EGFR mutation. Case Rep Oncol 2014;7(3):769–73. [CrossRef]
[Pubmed]

4.
Hsu F, Nichol A, Toriumi T, De Caluwe A. Miliary metastases are associated with epidermal growth factor receptor mutations in non-small cell lung cancer: A population-based study. Acta Oncol 2017;56(9):1175–80. [CrossRef]
[Pubmed]

5.
Sekine A, Katano T, Oda T, et al. Miliary lung metastases from non-small cell lung cancer with exon 20 insertion: A dismal prognostic entity: A case report. Mol Clin Oncol 2018;9(6):673–6. [CrossRef]
[Pubmed]

6.
Ramalingam SS, Yang JCH, Lee CK, et al. Osimertinib as first-line treatment of EGFR mutation-positive advanced non-small-cell lung cancer. J Clin Oncol 2018;36(9):841–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Waheed Abdul - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2022 Waheed Abdul. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.