|
Case Report
STUMPed. Is this a case of STUMP or a benign leiomyoma with extensive degenerative changes?
1 Department of Obstetrics & Gynaecology, Toowoomba Base Hospital, Queensland, Australia
2 Griffith University, Queensland, Australia
3 Royal Women’s Hospital, Melbourne, Australia
4 University of Queensland, Queensland, Australia
Address correspondence to:
Daina Waugh
Toowoomba Base Hospital, Toowoomba, QLD,
Australia
Message to Corresponding Author
Article ID: 101283Z01DW2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Waugh D, Lucky T, Abeysundera S. STUMPed. Is this a case of STUMP or a benign leiomyoma with extensive degenerative changes? Int J Case Rep Images 2022;13:101283Z01DW2022.ABSTRACT
Introduction: Smooth muscle tumors of uncertain malignant potential (STUMP) are rare uterine neoplasms that cannot be histologically identified as explicitly benign or malignant.
Case Report: This is a report on the case of a 43-year-old nulliparous woman with a multi-fibroid uterus initially indicating a smooth muscle tumor of uncertain malignant potential (STUMP) following hysterectomy. This case describes the investigation and management of symptomatic anemia secondary to menorrhagia in relation to a benign leiomyoma that was initially diagnosed as STUMP in a woman who did not desire fertility to be preserved.
Conclusion: Smooth muscle tumors of uncertain malignant potential can pose significant diagnostic and therapeutic challenges to clinicians, a carefully designed management and follow-up plan considering the patient factors is essential.
Keywords: Benign leiomyoma, Menorrhagia, STUMP, Tumor necrosis
Introduction
Smooth muscle tumors of uncertain malignant potential (STUMP) are rare uterine neoplasms that cannot be histologically identified as explicitly benign or malignant [1]. STUMP is a poorly defined subcategory of smooth muscle tumors that have further been subdivided into four histological groups based on atypia, mitotic figures, and necrosis. As STUMP cannot equivocally be defined as either leiomyoma, its variants or leiomyosarcoma is considered that it may represent a transition point between the two and thus raise concerns of the malignant potential and management options [2]. Due to the rarity and scarcity of data, a diagnosis of STUMP can be difficult and is made in approximately 0.01% in women who have undergone a myomectomy or a hysterectomy for a presumed diagnosis of leiomyoma [3]. With the limited data on incidence and recurrence, and in absence of clearly defined diagnostic features, STUMP in pre-menopausal women with or without fertility desire can pause significant diagnostic and therapeutic challenges to the treating clinicians. This case report describes surgical management of a pre-menopausal patient with leiomyoma with extensive degenerative changes that was initially histologically diagnosed as STUMP. We also review current literature to detail recent updates on diagnosis and management of STUMP.
Case Report
A 43-year-old Australian woman presented for a second time to the Emergency Department of Toowoomba Base Hospital for management of symptomatic anemia secondary to heavy menstrual bleeding. She had a history of regular 28-day cycles with 10 days of bleeding, heaviest in the first 3–4 days with occasional intermenstrual bleeding. Her recent pre-syncopal events secondary to anemia had improved post-iron infusion with her General Practitioner.
Over a period of four weeks prior to her presentation, the patient had commenced norethisterone, tranexamic acid, and mefenamic acid. This was on a background of taking oral iron supplements for years, being up to date with her cervical screening tests which were previously normal and having no other past medical or surgical history. She lives with her husband and both confirmed they do not desire children. She is a smoker of 15 cigarettes per day and uses no illicit drugs.
Examination revealed a well looking, hemodynamically stable and afebrile woman with a body mass index of 30. Her abdomen was soft and slightly tender in the left lower quadrant without rebound tenderness or guarding. Pelvic examination revealed a bulky, mobile, anteverted uterus with no adnexal masses felt.
At initial review in the Emergency Department her investigations discovered a hemoglobin of 83 g/L and a negative beta Human Chorionic Gonadotropin (bHCG). Remainder of the full blood count, liver function, kidney function, coagulation studies, and thyroid stimulating hormone were normal. Transabdominal ultrasound described a bulky, multi-fibroid, anteverted uterus with an endometrial thickness of 6.7 mm, a submucosal fibroid of 4.8 × 3.9 × 4.1 cm, otherwise normal ovaries and no intraperitoneal free fluid. A magnetic resonance imaging (MRI) may have been useful to further clarify the fibroid pre-operatively; however, this was not performed in this case.
A provisional diagnosis of abnormal uterine bleeding likely secondary to a multi-fibroid uterus and associated with symptomatic anemia was made. This patient was admitted for a blood transfusion and received one unit of packed red blood cells. She underwent a hysteroscopy, dilatation and curettage, and an intrauterine device (Mirena) insertion the following day. Multiple submucosal and intramural fibroids were visualized during the hysteroscopy; however, due to more than 50% myometrial involvement and a broad base of the largest fibroid it was deemed, not suitable for resection using a resectoscope. An endometrial curettage was performed and a Mirena inserted. Histology of the endometrial curettings identified secretory endometrium, negative for inflammation, hyperplasia, or malignancy.
During a post-operative review consultation, the patient was adamant that she did not desire her fertility to remain intact and preferred a hysterectomy as definitive management for her menorrhagia. She was appropriately counseled, consented, and a total laparoscopic hysterectomy, bilateral salpingectomy, excision of endometriosis, and cystoscopy was performed two months later. Endometriosis rAFS 1 (revised American Fertility Society) was identified and excised with monopolar scissors from the right pelvic side wall ovarian fossa and left side of the pouch of Douglas. Lesion at left uterovesical fold was removed with the hysterectomy specimen. The hysterectomy was overall uncomplicated and specimen was sent for histology. The vaginal cuff was closed with a 3-0 V-loc suture, cystoscopy was normal and estimated blood loss was 100 mL. Post-operative recovery was uncomplicated, and the patient was discharged two days later with a review was planned for 8–10 weeks post-operation.
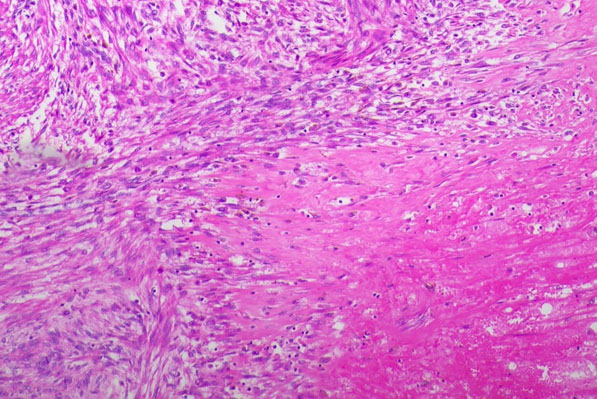
The initial post-operative histology confirmed endometriosis and initially reported STUMP, therefore a second opinion was sought. This further expert’s impression was that the equivocal necrosis was very likely degenerative in nature given the characteristic ischemic type effect and the relative paucity of atypia and mitotic activity, as seen Figure 1.
The second pathologist concluded that the degenerative cellular changes were keeping with hormonal therapy and a decision of benign leiomyoma with extensive degenerative changes was made rather than continuing with the initial diagnosis of STUMP, as seen in Figure 2.
The case was initially referred to the Gynaecology Oncology Tumour board at the Mater Hospital Brisbane when the histology indicated STUMP; however, following further experts’ opinion of a benign diagnosis, no Gynaecology Oncology intervention was required.
The patient was informed and reassured of the results and her post-surgical follow-up was unremarkable.
Discussion
Smooth muscle tumor of uncertain malignant potential encompasses a group of rare tumors with a reported incidence of only 0.01%. However, the statistics on the incidence or occurrence rate is based on the very limited data that are available in the literature. A limited number of large series studies and few case reports form the source of information on STUMP depicting its clinical behavior, recurrence rates, prognostic factors, and suggested long-term outcomes [4]. Therefore, ongoing reporting of this rare condition and regular review of the available literature by the treating clinicians is essential to optimize surgical management and postoperative follow-up.
Uterine smooth muscle tumors with unknown malignant potential usually range from leiomyomas to leiomyosarcomas. The three criteria that are used to histologically classify smooth muscle tumors as either benign or malignant include tumor necrosis, mitosis index, and nuclear atypia [1]. Tumor cell necrosis is a result of inadequate vascular supply and ensuing metabolic stressors within a tumor, the mitosis index is a measure of the proliferation status of a cell population and is measured in mitotic figures/10 high powered fields (HPF), for STUMP this is widely categorized as <10/10 HPF [1]. Nuclear atypia describes atypical features of the nuclei including size and irregularity and is classified as mild to severe.
To diagnose the tumor as malignant, at least two of the three criteria need to be met. A uterine smooth muscle tumor is diagnosed as STUMP when only one of the three criteria is met for malignancy [2]. In our patient, the only defining criterion was the tumor necrosis as there was a relative lack of atypia and mitotic activity. The pathologist accepted that equivocal necrosis, that of tumor type versus ischemic, can be placed in the STUMP category; however, continued to conclude that this necrosis could also be likely from the degenerative changes secondary to hormonal therapy rather than the tumor type. This eventually leads to a conclusion of benign leiomyoma.
This is the first case report to detail a finding of leiomyoma with degenerative changes that initially was diagnosed as STUMP. There is currently further research evolving around the diagnostic criteria of STUMP. Based off the currently accepted WHO guidelines, Gupta et al. have proposed a redefinition of the diagnostic criteria [5]. For this patient, the proposed redefinition would not affect her outcome or follow-up, as the presence of necrosis was not particularly associated with adverse outcomes. Gupta et al. propose that other criteria such as atypical mitosis, epithelioid differentiation, vascular involvement, and irregular margins be considered in the diagnostic criteria.
One of the commonest presentations of uterine smooth muscle tumors is abnormal uterine bleeding (AUB), particularly in the form of heavy menstrual bleeding (HMB) and associated secondary outcomes such as iron deficiency anemia, requirement of iron and and/or blood transfusion and recurrent hospitalization. This array of presentations was also reflected in our case. Currently, hormonal therapy is one of the first line treatments and widely used for women experiencing HMB with and without smooth muscle tumors [6]. In our case, an intrauterine with levonorgestrel releasing system (Mirena) was inserted during the initial evaluation with hysteroscopy and endometrial biopsy. Mirena remained in situ for approximately two months prior to the hysterectomy to help reduce blood loss and risk of anemia pre-hysterectomy. First line therapies taking into account her age and smoking status were utilized prior to the Mirena in this case without cessation or reduction of bleeding and therefore surgical management options were explored and utilized. However, it is important to recognize that the overall management strategy for symptomatic uterine smooth muscle tumors widely varies based on patient factors (i.e., symptom profile, menopausal status, fertility wishes, presence of other co-morbidities, surgical fitness, etc) and beyond the scope of this report [7].
The follow-up between STUMP and leiomyoma is widely different, with a benign leiomyoma diagnosis requiring only regular post-surgical follow-up and comes with no risk of recurrence following a hysterectomy. The recurrence rates of STUMP can range between 8.7% and 11% [3]; however, these statistics are based on a very limited number of studies and case reports. Thus, due to its rarity and lack of robust evidence, no standard protocols for the management or follow-up of STUMP is currently available. Smooth muscle tumors of uncertain malignant potential may recur as either STUMPs itself or leiomyosarcomas. Recurrent cases need surgical excision and depending on individual circumstances may also need subsequent adjuvant radiotherapy, chemotherapy, and hormonal therapies [2]. In their case report, Shapiro et al. [8] detailed the current controversies and dilemmas on diagnosis, management strategies, and undefined prognosis of STUMP.
Given the limited literature, there is also no consensus regarding clinical characteristics of recurrence. Anatomical sites, timing, and histological type have yet to be defined. Atkins et al. [9] reported three cases of recurrence with metastatic disease following initial management; these included peritoneal, lymph node, and liver metastases. Further management included progesterone and surgical tumor debulking. Dall’Asta et al. [2] described a five case STUMP study recommending six monthly clinical evaluation in patients who underwent hysterectomy followed by yearly computed tomography scan. For patients who decide on maintaining fertility, a more frequent monitoring schedule is required. In our case, the patient was counseled on the differences between STUMP and benign leiomyoma following the initial diagnosis and will continue with her post-surgical follow-up as planned with a review 12 weeks post-surgery.
Conclusion
Smooth muscle tumors of uncertain malignant potential can pose significant diagnostic and therapeutic challenges to clinicians especially when the diagnosis is made in operative specimens from reproductive-age women. A carefully designed management and follow-up plan considering the patient factors is essential. Clinicians should familiarize themselves with the underlying pathology of STUMP and routinely review the literature to remain up to date with recommended management options and follow-up to optimize patient’s course of treatment.
REFERENCES
1.
2.
Dall'Asta A, Gizzo S, Musarò A, et al. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): Pathology, follow-up and recurrence. Int J Clin Exp Pathol 2014;7(11):8136–42.
[Pubmed]

3.
Ip PPC, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: A review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol 2010;17(2):91–112. [CrossRef]
[Pubmed]

4.
Conte AB, Elhaoudani J, Yessoufou M, Chaara H, Melhouf AM. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): Management, follow up and prognosis. PAMJ Clinical Medicine 2020;3(82). [CrossRef]

5.
Gupta M, Laury AL, Nucci MR, Quade BJ. Predictors of adverse outcome in uterine smooth muscle tumours of uncertain malignant potential (STUMP): A clinicopathological analysis of 22 cases with a proposal for the inclusion of additional histological parameters. Histopathology 2018;73(2):284–98. [CrossRef]
[Pubmed]

6.
Maybin JA, Critchley HOD. Medical management of heavy menstrual bleeding. Womens Health (Lond) 2016;12(1):27–34. [CrossRef]
[Pubmed]

7.
Munro MG, Critchley HO, Broder MS, Fraser IS; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet 2011;113(1):3–13. [CrossRef]
[Pubmed]

8.
Shapiro A, Ferenczy A, Turcotte R, Bruchim I, Gotlieb WH. Uterine smooth-muscle tumor of uncertain malignant potential metastasizing to the humerus as a high-grade leiomyosarcoma. Gynecol Oncol 2004;94(3):818–20. [CrossRef]
[Pubmed]

9.
Atkins KA, Arronte N, Darus CJ, Rice LW. The use of p16 in enhancing the histologic classification of uterine smooth muscle tumors. Am J Surg Pathol 2008;32(1):98–102. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
Darling Downs Health
Author ContributionsDaina Waugh - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tarana Lucky - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Senaka Abeysundera - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent has been provided by the patient for this case reports publication.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Daina Waugh et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.