|
Case Report
“Dropped head syndrome” in amyotrophic lateral sclerosis: A case report
1 Medical Student and Member of the Editorial Team of the Journal of Biological and Health Sciences of the Universidade Iguaçu, Nova Iguaçu, Rio de Janeiro, Brazil
2 Physician, Post-Doctorate in Health Sciences, Doctor in Neurology, Master in Collective Health, Professor and Coordinator of the Master's Degree Program in Neurology at the University of Vassouras and Adjunct Professor at the Medical School of the Iguaçu University, Rio de Janeiro, Brazil
3 Iguaçu University – UNIG – Hospital Geral de Nova Iguaçu, Rio de Janeiro, Brazil
Address correspondence to:
Antônio Marcos da Silva Catharino
Rua Gavião Peixoto 70, Room 811, CEP 24.2230-100, Icaraí, Niterói-RJ,
Brazil
Message to Corresponding Author
Article ID: 101274Z01JN2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
do Nascimento JF, Orsini M, Rodrigues ASP, Leitão RM, Nunes NSM, da Silva Catharino AM. “Dropped head syndrome” in amyotrophic lateral sclerosis: A case report. Int J Case Rep Images 2021;12:101274Z01JN2021.ABSTRACT
Introduction: The dropped head syndrome (DHS), also called slack head syndrome, was first detailed in 1986. This condition was recognized in 12 patients with various neuromuscular disorders, such as amyotrophic lateral sclerosis (ALS). It is characterized by asthenia of the extensor musculature of the neck, with or without asthenia of the flexor musculature of the neck, causing an inability to condition the head support and leading patients to the typical aspect of the flexed head with the chin in contact with the thoracic region.
Case Report: We report the case of a 68-year-old female who diagnosed with amyotrophic lateral sclerosis (ALS) about two years ago and reported limitations in her daily activities as the disease progressed. In her last visit, dated 03/30/2021, she presented great difficulty in sustaining her head in an anti-gravity position and, when asked to “bend” this region, she was unsuccessful in reerecting it. Need of concentration to maintain the cervical in neutral position and, after minutes, presented extreme fatigue with melting.
Conclusion: Despite being uncommon in ALS, the dropped head syndrome may occur in early or late stages and cause severe consequences to the individual, increasing his dependence and limiting his social interaction and quality of life. Given its numerous etiologies, patients with DHS without an established diagnosis should be investigated for the possible diagnosis of ALS. Measures are essential to prevent the installation of fixed deformities and the early designation of the best therapeutic approach for the patient becomes crucial.
Keywords: Amyotrophic lateral sclerosis, Electroneuromyography, Motor neuron
Introduction
The dropped head syndrome (DHS), also called slack head syndrome, was first detailed in 1986. This condition was recognized in 12 patients with various neuromuscular disorders, such as amyotrophic lateral sclerosis (ALS). It is characterized by asthenia of the extensor musculature of the neck, with or without asthenia of the flexor musculature of the neck, causing an inability to condition the head support and leading patients to the typical aspect of the flexed head with the chin in contact with the thoracic region (Figure 1) [1],[2].
Different etiologies are related to droopy head syndrome, and this is also a condition that presents in isolation. The first reports occurred in patients affected by myasthenia gravis, motor neuron disease, polymyositis, sclerodermatomyositis, and facioscapulohumeral dystrophy (FSHD), as well as isolated paralysis of the head extensors, Parkinson's disease, Duchenne muscular dystrophy, and progressive myotrophy. In 1992, Suarez and Kelly [2] evidenced in their study a non-inflammatory myopathy that essentially affected the extensor muscles of the neck. From this, DHS was named as a new clinical disorder, characterized by significant asthenia in the neck extensors, with diminished loss of strength in the scapular girdle and proximal arm muscles [3],[4].
Despite the impairments caused by DHS, these are rarely described in patients impaired by motor neuron disease. Although the pathophysiological mechanism of DHS in amyotrophic lateral sclerosis is not completely elucidated, it is believed to be a consequence of the impairment of the motor neuron body located at the anterior end of the spinal cord, which is responsible for innervating the paraspinal muscles [3],[5].
The objective of the present study is to discuss the case of a patient who, approximately two years after the onset of the disease, presented DHS and, as a consequence, several moderations with regard to social integration and functional abilities.
Case Report
We report the case of a 68-year-old female who diagnosed with amyotrophic lateral sclerosis (ALS) about two years ago and reported limitations in her daily activities as the disease progressed. In her last visit, dated 03/30/2021, she presented great difficulty in sustaining her head in an anti-gravity position and, when asked to “bend” this region, she was unsuccessful in reerecting it. Need of concentration to maintain the cervical in neutral position and, after minutes, presented extreme fatigue with melting. Myoarticular pain in the region surrounding the cervical spine signals a possible “overload.” Although dysphagia and dyspnea problems have not yet been the cause of complaints, the patient is fearful about the abrupt evolution of the disease and apprehensive about not being able to perform movements in this region. She is tetraparetic, with abolished deep reflexes, bilateral Hofmann’s sign, and full of fasciculations in the four limbs.
Discussion
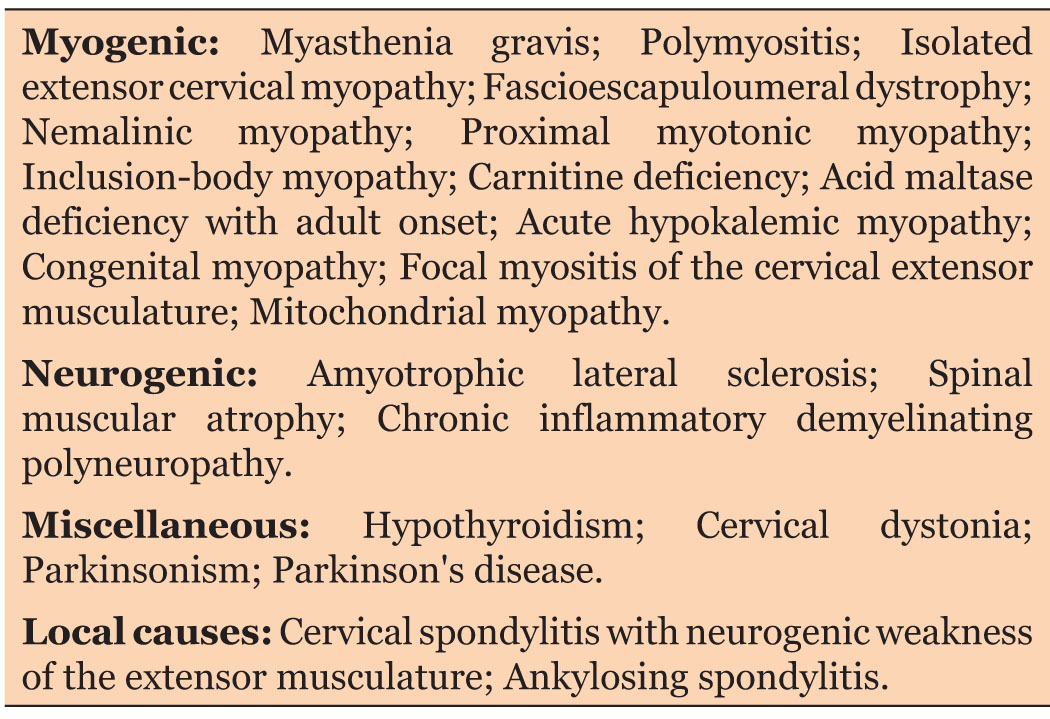
Asthenia of the extensor musculature of the neck, in the absence or not of involvement of the flexor muscles, leading to the development of DHS, may be caused by several etiologies. Gourie-Devi et al. [6] proposed an etiological classification, dividing patients into different groups according to the condition in question: myogenic, neurogenic, miscellaneous, and local (Table 1). Among the causes of DHS, neuromuscular diseases are little described in the literature. Also in their research, Gourie-Devi et al. (2003) [6] studied a quantitative of 683 patients with ALS of which only 9 (1.3%) had seen a DHS, demonstrating the rarity of this manifestation in these individuals [6].
The initial symptoms of ALS commonly occur in the muscles of the lower and upper limbs, as well as the bulbar muscles. The asthenia seen in the muscles of the neck and trunk is the first symptom in only 2% of the cases of ALS [7]. Involvement of the flexor musculature of the neck occurs frequently, however, the succession of extensor paresis with subsequent melting of the head is uncommon. Dropped head syndrome manifests itself in the early stages, this occurs around 3–24 months after the diagnosis is made, in the late stages, it occurs around 3–8 years after the diagnosis [6].
Some complementary exams are necessary for the investigation of DHS, which are selected according to the researched etiology. Electroneuromyography (ENMG) is considered a gold standard complementary exam for providing direction for investigation among neurogenic, myogenic, and neuromuscular junction diseases. To date, there are no imaging studies associated with ALS [5].
Dropped head syndrome can present as an extremely disabling condition, causing difficulty in pronouncing words, dyspnea, and spinal cord injuries secondary to traction. If present, significant paresis of the extensor musculature may favor the development of instabilities of the cervical spine [8]. The involvement of the bulbar muscles results in dysphagia, which can be aggravated by DHS. In view of this, the attenuation of such symptom can happen through the use of head supports [6]. In some cases respiratory failure develops due to an inability to control the upper airway. Furthermore, external factors such as intimidation imposed by society need special attention, and this can be corrected by the use of a neck brace [9].
The treatment requires a multidisciplinary team, where delicate and careful attention must be given to the complications and comorbidities that patients may present. The determination of the type of DHS that the patient presents, as well as its etiology, is fundamental for the choice of the best therapeutic approach to be determined. As to the type, when it is flexible, there is the possibility of correction through passive extension of the head [10], which is done through the use of cervical collars, associated with rehabilitation treatment performed by a physiotherapist, thus enabling an improvement in posture and facilitating the individual’s daily actions and socialization, which is the approach indicated for patients with ALS [4], such as the patient reported in this case.
In cases where the deformity is fixed and passive correction is not possible, or even in cases of failure of the aforementioned therapy, a surgical approach can be indicated for correction of the DHS, providing the patient with long-term stabilization [8] with posterior fusion, combined anteroposterior, and cervical pedicle subtraction osteotomy being some of the surgical options to be adopted. However, it is noteworthy that there is a limitation in the literature when it comes to the surgical approach to the syndrome, requiring further studies to better demonstrate the effectiveness of these procedures [11].
Conclusion
Despite being uncommon in ALS, the drooped head syndrome may occur in early or late stages and cause severe consequences to the individual, increasing his dependence and limiting his social interaction and quality of life. Given its numerous etiologies, patients with DHS without an established diagnosis should be investigated for the possible diagnosis of ALS. Measures are essential to prevent the installation of fixed deformities and the early designation of the best therapeutic approach for the patient becomes crucial.
REFERENCES
2.
Suarez GA, Kelly JJ Jr. The dropped head syndrome. Neurology 1992;42(8):1625–7. [CrossRef]
[Pubmed]

3.
4.
Burakgazi AZ, Richardson PK, Abu-Rub M. Dropped head syndrome due to neuromuscular disorders: Clinical manifestation and evaluation. Neurol Int 2019;11(3):8198. [CrossRef]
[Pubmed]

5.
Lorenzoni PJ, Lange MC, Kay CSK, et al. Dropped head syndrome in motor neuron disease. [Article in Portuguese]. Arq Neuropsiquiatr 2006;64(1):118–21. [CrossRef]
[Pubmed]

6.
Gourie-Devi M, Nalini A, Sandhya S. Early or late appearance of “dropped head syndrome” in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 2003;74(5):683–6. [CrossRef]
[Pubmed]

7.
Jokelainen M. Amyotrophic lateral sclerosis in Finland. II: Clinical characteristics. Acta Neurol Scand 1977;56(3):194–204. [CrossRef]
[Pubmed]

8.
Nakanishi K, Taneda M, Sumii T, Yabuuchi T, Iwakura N. Cervical myelopathy caused by dropped head syndrome. Case report and review of the literature. J Neurosurg Spine 2007;6(2):165–8. [CrossRef]
[Pubmed]

9.
10.
Taniguchi S, Takahashi H, Aoki Y, et al. Surgical treatment for dropped head syndrome with cervical spondylotic amyotrophy: A case report. BMC Res Notes 2018;11(1):500. [CrossRef]
[Pubmed]

11.
Marcon RM, Ono AHA, Zelada FGB, Cristante AF, Barros TEP. Surgical correction of severe and fixed chin-on-chest deformity. Acta Ortop Bras 2018;26(6):415–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jacqueline Fernandes do Nascimento - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marco Orsini - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Angélica Sabino Pereira Rodrigues - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Roberto Monteiro Leitão - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nicolle dos Santos Moraes Nunes - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Antônio Marcos da Silva Catharino - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Jacqueline Fernandes do Nascimento et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.