|
Case Report
Recurrent inguinal abscess revealing chronic appendicitis: A case report and review of the literature
1 Resident, Radiology, Military Hospital, Rabat, Morocco
2 Professor, Radiology, Military Hospital, Rabat, Morocco
3 Professor and Department Chief, Radiology, Military Hospital, Rabat, Morocco
Address correspondence to:
Iraqi Fatima Zahra
Resident, Radiology, Military Hospital, Agdal, Rabat,
Morocco
Message to Corresponding Author
Article ID: 101269Z01IZ2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Fatima Zahra I, Kebir DM, Hassan N, Jamal EF. Recurrent inguinal abscess revealing chronic appendicitis: A case report and review of the literature. Int J Case Rep Images 2021;12:101269Z01IZ2021.ABSTRACT
Introduction: Chronic appendicitis is currently defined as a long standing inflammation of the appendix that presents clinically as prolonged (>48 hours) or intermittent abdominal pain. Its diagnosis is often only made after appendectomy and histological analysis of the appendix. This condition may lead to serious consequences as abscess formation.
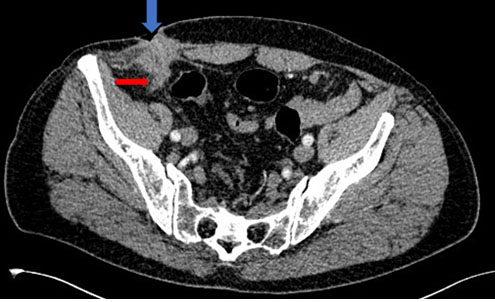
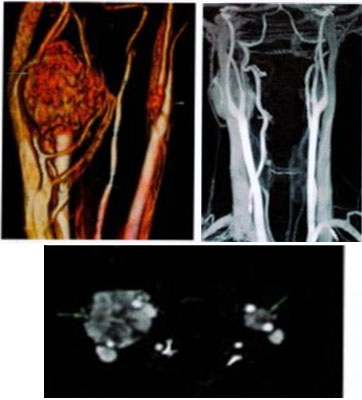
Case Report: We report the case of a 64-year-old patient who had been operated for a recurrent right inguinal hernia on several occasions and had presented for two years an issue of purulent fluid through the open scar. An abdomino-pelvic computed tomography (CT) scan was requested to look for a potential digestive fistula. It showed a heterogeneous thickening of the hernia scar spread over 39 mm, poorly limited, containing calcification with infiltration of fat around. This infiltration was in contact with the distal end of the appendix which was thickened. We concluded to the diagnosis of chronic appendicitis.
Conclusion: Chronic appendicitis is a diagnosis characterized by long-standing lower quadrant pain that is associated with histopathologic chronic inflammatory changes. We must evoke this diagnosis in front of any recurrent inguinal abscess.
Keywords: Abscess, Chronic appendicitis, Inguinal hernia
Introduction
Acute appendicitis is an acute inflammation of the appendix created by a luminal blockage of external origin as a lymphoid hyperplasia or internal by materials or a stercolith [1].
Clinically, it manifests as umbilical pain migrating to the right lower quadrant, dating less than 48 hours and is associated with abdominal defense, fever, anorexia, nausea, vomiting, lethargy, elevated inflammatory markers and tenderness in McBurney point [2],[3].
In regard to chronic appendicitis, it’s a rare disease that is difficult to diagnose. It was first reported by Crymble and Forsythe in 1949 [4], as a condition with at least 1 attack of mild appendicitis occurring in a sequence that may include more severe attacks [5].
It is currently defined as a long standing inflammation of the appendix that presents clinically as prolonged (>48 hours) or intermittent abdominal pain [6],[7].
Moreover, its diagnosis is often only made after appendectomy and histological analysis of the appendix [6].
Computed tomography imaging is considered the test of choice for patients with an equivocal presentation [8]. The diagnosis should not be missed because serious consequences may occur as abscess formation [9], occlusions or perforation [5].
Case Report
We report the case of a 64-year-old patient who had been operated for a recurrent right inguinal hernia on several occasions and had presented for two years an issue of purulent fluid through the open scar. The last hernia repair was done three years ago under laparotomy with inguinal incision using the Lichtenstein technique which consists in closing the inguinal opening with a light prosthesis after hernia reduction.
The patient had no comorbidities. His general condition was well, and his body temperature was 38.5°C. Physical examination revealed swelling, redness, local temperature increase and pain in the right inguinal region .Blood biochemistry values were normal. White blood cell count was 12,000/mm3,and C-reactive protein level was 40 mg/L. Taking into account his surgical history, an abdomino-pelvic CT scan was requested to look for a potential digestive fistula.
The CT showed an heterogeneous thickening of the hernia scar spread over 39 mm (Figure 1), poorly limited, containing calcification (Figure 2) with infiltration of fat around (Figure 3).
This infiltration was in contact with the distal end of the appendix which was thickened (Figure 1).
Liver, spleen, kidneys, and pancreas were without abnormalities. No deep lymphadenopathy or peritoneal effusion was found.
We concluded to a right inguinal collection continuing with the appendix which was thickened, in favor of chronic appendicitis.
The current surgery was performed under laparotomy with inguinal incision on the previous scar. An abscessed collection of thick liquid was revealed, it was in contact with the swollen appendix. The mesh previously used for the hernia repair appeared to be affected by the infection due to its dirty appearance; it was therefore removed and replaced.
Appendectomy and abscess drainage were performed and the patient was put under observation for a few days.
Discussion
The incidence rate of chronic appendicitis is estimated at 1.5% of all cases in general population [8]. This condition is difficult to diagnose for clinicians because patients do not present typical signs of appendicitis. There are also no formal criteria for this kind of appendicitis [8],[9]. Its diagnosis is generally made after an appendectomy and based on histologic findings of chronic inflammatory changes [5], such as fibrosis, lymphoplasmocytic inflammatory infiltrate, and a prevalence of T lymphocytes [10],[11].
The physiopathology of chronic or recurrent appendicitis is yet to be discussed [7]. For some authors it is due to a mechanical partial obstruction of the appendix lumen which leads to a gradual distension of the appendix wall [12]. For others, it is due to an excessive production of mucus within the appendix lumen [13].
Clinically, most patients report a moderate right lower quadrant abdominal pain lasting more than 48 hours. It could last up for months or years or could be a recurrent episodic pain [14],[15]. It can be present with or without associated systemic symptoms and the laboratory test results might be normal [16].
The management of chronic appendicitis is based on surgical exploration followed by an appendectomy if no other obvious pathology is identified [17],[18],[19]. Most of the studies describe a relief of symptoms few years after appendectomy, particularly in children [20],[21].
Although it is not considered as a surgical emergency, for most patients with chronic appendicitis, resolution of pain comes with appendectomy [8].
Imaging studies might be helpful in the diagnosis of chronic appendicitis [5]. Ultrasound is used first, and if it is not helpful, we go to CT scan, or endoscopy [8]. Magnetic resonance imaging (MRI) should be considered in pediatric population [22]. Computed tomography may find pericecal stranding, dilated appendix, apical thickening, adenopathy, appendicolith, abscess, arrowhead sign, phlegmon, and fluid [8].
Hernia is a general term describing a protrusion of an organ or tissue through an abnormal opening within the anatomic structure. 75% of all hernias occur in the inguinal region with 9:1 male predominance [23].
It would be interesting to cite Amyand hernia as an example of an association between inguinal hernia and appendicitis, and a condition that should be considered in cases of recurrent inguinal abscess [24]. It is a rare event described by an acute or perforated appendicitis occurring within an inguinal hernia [25]. Indeed, the appendix is found in the hernial sac during surgery.
The first case was reported in 1735 by the surgeon Claudius Amyand in an 11-year-old-male patient [25]. It is said to occur secondary to ischemic events related to incarceration because of the sedation and analgesia used for the manual reduction of the incarcerated hernia and/or direct trauma to the appendix during that reduction [26].
Conclusion
Appendiceal inflammation can sometimes occur in a chronic form. Chronic appendicitis is a diagnosis characterized by long-standing lower quadrant pain that is associated with histopathologic chronic inflammatory changes. This condition may lead to serious complications as abscess formation, occlusion, and perforation. Appendectomy improves symptoms in most patients. Any recurrent inguinal abscess should suggest the diagnosis of chronic appendicitis in addition to complications due to the type of hernia repair therapy such as hernia mesh infection.
REFERENCES
2.
3.
Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE. Does this child have appendicitis? JAMA 2007;298(4):438–51. [CrossRef]
[Pubmed]

4.
Crymble PT, Forsythe I. Chronic appendicitis in children. Ulster Med J 1949;18(2):153–72.2.
[Pubmed]

5.
Kim D, Butterworth SA, Goldman RD. Chronic appendicitis in children. Can Fam Physician 2016;62(6):e304–5.
[Pubmed]

6.
7.
Mattei P, Sola JE, Yeo CJ. Chronic and recurrent appendicitis are uncommon entities often misdiagnosed. J Am Coll Surg 1994;178(4):385–9.
[Pubmed]

8.
Shah SS, Gaffney RR, Dykes TM, Goldstein JP. Chronic Appendicitis: An often forgotten cause of recurrent abdominal pain. Am J Med 2013;126(1):e7–8. [CrossRef]
[Pubmed]

9.
Mueller BA, Daling JR, Moore DE, et al. Appendectomy and the risk of tubal infertility. N Engl J Med 1986;315(24):1506–8. [CrossRef]
[Pubmed]

10.
Panchalingam L, Driver C, Mahomed AA. Elective laparoscopic appendicectomy for chronic right iliac fossa pain in children. J Laparoendosc Adv Surg Tech A 2015;15(2):186–9. [CrossRef]
[Pubmed]

11.
Paredes Esteban RM, Salas Molina J, Ocaña Losa JM, Jaime BE. Indication of appendectomy in the recurrent abdominal pain. [Article in Spanish]. Cir Pediatr 2004;17(2):65–9.
[Pubmed]

12.
Homer MJ, Braver JM. Recurrent appendicitis: Reexamination of a controversial disease. Gastrointest Radiol 1979;4(3):295–301. [CrossRef]
[Pubmed]

13.
Seidman JD, Andersen DK, Ulrich S, Hoy GR, Chun B. Recurrent abdominal pain due to chronic appendiceal disease. South Med J 1991;84(7):913–6. [CrossRef]
[Pubmed]

14.
Rao PM, Rhea JT, Novelline RA, McCabe CJ. The computed tomography appearance of recurrent and chronic appendicitis. Am J Emerg Med 1998;16(1):26–33. [CrossRef]
[Pubmed]

15.
16.
Van Winter JT, Wilkinson JM, Goerss MW, Davis PM. Chronic appendicitis: Does it exist? J Fam Pract 1998;46(6):507-9.
[Pubmed]

17.
Hawes AS, Whalen GF. Recurrent and chronic appendicitis: The other inflammatory conditions of the appendix. Am Surg 1994;60(3):217–9.
[Pubmed]

18.
Crabbe MM, Norwood SH, Robertson HD, Silva JS. Recurrent and chronic appendicitis. Surg Gynecol Obstet 1986;163(1):11–3.
[Pubmed]

19.
Moore MM, Gustas CN, Choudhary AK, et al. MRI for clinically suspected pediatric appendicitis: An implemented program. Pediatr Radiol 2012;42(9):1056–63. [CrossRef]
[Pubmed]

20.
Kolts RL, Nelson RS, Park R, Heikenen J. Exploratory laparoscopy for recurrent right lower quadrant pain in a pediatric population. Pediatr Surg Int 2006;22(3):247–9. [CrossRef]
[Pubmed]

21.
Stringel G, Berezin SH, Bostwick HE, Halata MS. Laparoscopy in the management of children with chronic recurrent abdominal pain. JSLS 1999;3(3):215–9.
[Pubmed]

22.
Checkoff JL, Wechsler RJ, Nazarian LN. Chronic inflammatory appendiceal conditions that mimic acute appendicitis on helical CT. AJR Am J Roentgenol 2002;179(3):731–4. [CrossRef]
[Pubmed]

23.
LeBlanc KE, LeBlanc LL, LeBlanc KA. Inguinal hernias: Diagnosis and management. Am Fam Physician 2013;87(12):844–8.
[Pubmed]

24.
Tartar T, Saraç M, Bakal Ü, Onur MR, Kazez A. A rare cause of inguinal sabscess: Perforated appendicitis due to foreign body in Amyand’s hernia. Turk J Pediatr 2020;62(5):889–92. [CrossRef]
[Pubmed]

25.
Yazici M, Etensel B, Gürsoy H, Ozkisacik S, Erkus M, Aydin ON. Infantile Amyand’s hernia. Pediatr Int 2003;45(5):595–6. [CrossRef]
[Pubmed]

26.
Hennington MH, Tinsley EA, Proctor HJ, Baker CC. Acute appendicitis following blunt abdominal trauma. Incidence or coincidence? Ann Surg 1991;214(1):61–3. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Iraqi Fatima Zahra - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Daoud Ali Mohamed - Acquisition of data, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nouali Hassan - Conception of the work, Design of the work, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
El Fenni Jamal - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Iraqi Fatima Zahra et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.