|
Case Report
Pleomorphic adenoma in buccal mucosa: A case report
1 DDS, Department of Oral Surgery, Mato Grosso Cancer Hospital, Cuiabá, MT, Brazil
2 DDS, MSc, PhD, Cuiabá Dental School, University of Cuiabá, Department of Oral Surgery, Mato Grosso Cancer Hospital, Cuiabá, MT, Brazil
Address correspondence to:
Luiz Evaristo Ricci Volpato
Universidade de Cuiabá, Av. Beira Rio, 3100 Jardim Europa, Cuiabá, MT, CEP: 78065-443,
Brazil
Message to Corresponding Author
Article ID: 101209Z01RA2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Afonso RAS, Godinho GV, de Nápoles Albuquerque BB, Volpato LER. Pleomorphic adenoma in buccal mucosa: A case report. Int J Case Rep Images 2021;12:101209Z01RA2021.ABSTRACT
Introduction: Pleomorphic adenoma is one of the most common salivary gland neoplasms, with the parotid gland being the most affected site and a lower incidence in the minor salivary glands. This article reports an unusual clinical case of pleomorphic adenoma of minor salivary gland, located in the buccal mucosa and presents its treatment.
Case Report: A 65-year-old female patient with a lesion in the buccal mucosa with evolution of approximately two years was evaluated. The anatomopathological report after incisional biopsy indicated pleomorphic adenoma. The treatment performed was a complete excision of the lesion under local anesthesia. The specimen, measuring 20.51 mm, was sent for anatomopathological examination, whose report confirmed the previous diagnosis.
Conclusion: The complete excision of pleomorphic adenoma of minor salivary gland in the buccal mucosa under local anesthesia allowed the patient to heal and prevented a possible malignant transformation, with little associated morbidity.
Keywords: Mouth mucosa, Pleomorphic adenoma, Surgical procedure, Treatment
Introduction
Pleomorphic adenoma is a common salivary gland neoplasm, with the parotid gland being the most affected site, and a lower incidence in the minor salivary glands. As for the incidence of pleomorphic adenoma, it is higher in adults aged between 30 and 60 years, with a higher rate of involvement in females [1].
Clinically, an ovoid, fixed, painless slow growth is observed, firm to palpation with well-defined margins, ranging from a few millimeters to several centimeters [2]. Complementary imaging tests (computed tomography, magnetic resonance imaging, and ultrasonography) offer tools for characterizing the lesion, assist in early diagnosis, treatment and, consequently, a better prognosis [3].
Treatment for pleomorphic adenoma of minor salivary glands consists of conservative enucleation. This treatment modality has an excellent prognosis when adequate surgical removal is performed, with low rates of recurrence and rare malignant transformation [4],[5]. Carcinoma ex-pleomorphic adenoma is rare, developing from about 6% of cases of pleomorphic adenoma [6].
In this sense, this work reports a clinical case of pleomorphic adenoma of minor salivary gland in the buccal mucosa and presents the technique used to remove the tumor in this unusual location.
Case Report
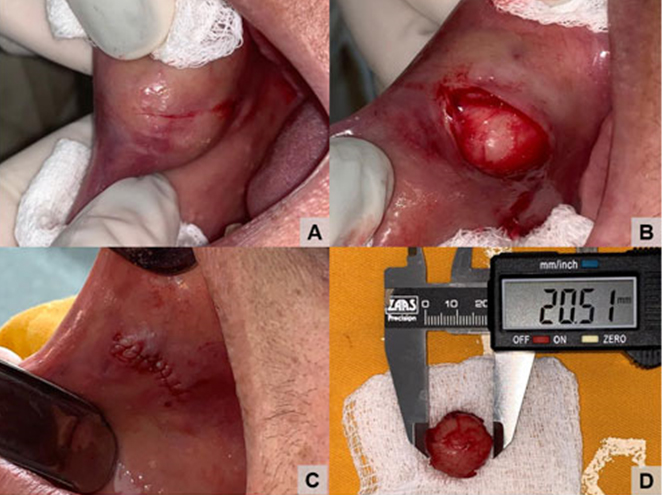
A 65-year-old female patient was referred to the Oral and Maxillofacial Surgery outpatient clinic of the Mato Grosso Cancer Hospital for evaluation of a lesion in the buccal mucosa, with an evolution of approximately two years. In her past medical history, the patient denied the use of any medication for continuous use, alcoholism, smoking, and history of head and neck radiation. In the intraoral clinical examination, a nodular lesion was observed in the left buccal mucosa, of a borrachoid consistency on palpation, mobile, with well-delimited margins and overlying, normal colored mucosa (Figure 1).
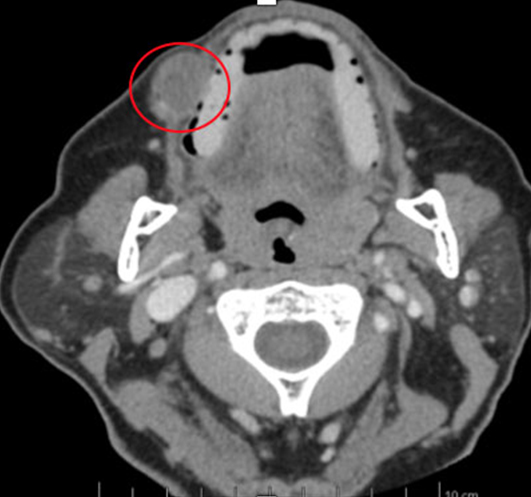
The team requested soft tissue ultrasound to determine clinical conduct. A nodule could be observed in the subcutaneous tissue of the right buccinator region, with well-defined and slightly lobulated limits, with apparent hyperechogenic bundle in its central portion, and with vascularization inside, measuring 2.1 × 1.3 × 1.4 cm. Subcutaneous cellular tissue was of normal echographic appearance and musculature was also of normal appearance and texture. The tomographic examination presented a hyperdense lesion in the region of the right buccal mucosa, between the buccinator muscle and the intraoral mucosa (Figure 2).
From the clinical and imaging exams, the diagnostic hypotheses were pleomorphic adenoma, fibroma, lipoma, and malignant neoplasms such as mucoepidermoid carcinoma, adenocarcinoma, cystic adenomatoid carcinoma and acinar cell carcinoma.
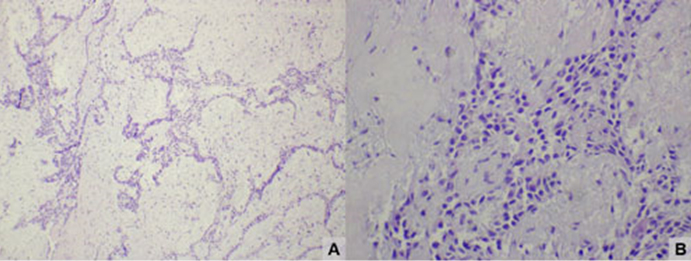
In view of this, an incisional biopsy was planned under local anesthesia. The anatomopathological report indicated pleomorphic adenoma, characterized by anatomical tubular structures and small cysts, constituted by cuboidal epithelial cells, with regular nuclei and pink cytoplasm, without atypias, amid chondromyxoid stroma with absence of malignancy and preserved adjacent glandular tissue (Figure 3).
The treatment performed was complete excision of the lesion under local anesthesia. An incision was made in the mucosa overlying the lesion, preventing rupture of the tumor capsule. This was followed by complete tissue divulsion, preserving the integrity of the surgical specimen. Copious irrigation was performed with 0.9% saline and sutured with Vicryl 5-0 thread. The piece, measuring 20.51 mm, was sent for anatomopathological examination, whose report confirmed the previous diagnosis of pleomorphic adenoma (Figure 4). The patient was discharged after the procedure. She was stable and oriented. There was no postoperative complication.
The patient is undergoing clinical follow-up for one year with no changes indicative of recurrence and with a satisfactory healing aspect (Figure 5).
Discussion
This case describes the diagnosis and treatment of a pleomorphic adenoma in the buccal mucosa. This is an unusual case since this lesion most commonly affects the parotid gland (70% of cases) [7] and when minor salivary glands are involved (5–25% of cases) [8], usually the lip and palate are the regions of highest occurrences [9].
Pleomorphic adenoma is the most common benign tumor of the salivary glands. The 2-year clinical evolution observed in the present case may be related to the fact that the pleomorphic adenoma is an asymptomatic tumor and has a slow evolution [10]; however, it has the possibility of becoming a malignant lesion such as carcinoma ex pleomorphic adenoma (about 6% of the cases [6]) that can present itself, asymptomatic and clinically similar to the benign form [11].
Diagnostic hypotheses were pleomorphic adenoma, fibroma, lipoma, in addition to malignant neoplasms such as mucoepidermoid carcinoma, adenocarcinoma, cystic adenomatoid carcinoma and acinic cell carcinoma [12]. It is worth mentioning that malignant salivary gland tumors can present clinically with an aspect of benignity and minor salivary gland tumors are predominantly malignant [13], thus complementary tests, such as fine needle aspiration or incisional biopsy, are usually used to define the diagnosis [14]. The fine needle aspiration biopsy has insufficient sensitivity and precision for the diagnosis of malignancy of pleomorphic adenoma, so the histopathological examination is more suitable for this purpose [15]. Although the incisional biopsy technique involves rupture of the tumor capsule, due to its greater sensitivity compared to the fine needle aspiration biopsy, it was the technique chosen to assist in the diagnosis of the lesion in the case presented.
Imaging examinations of computed tomography and ultrasound were also used in the present case in order to allow a more accurate diagnosis and consequently surgical planning with greater predictability [16].
The histopathological aspect of pleomorphic adenoma is characterized by a composition of epithelial, myoepithelial, and mesenchymal elements, surrounded by a myxoid, chondroid, or osteoid stroma [17],[18]. This aspect was found in this case, which presented cuboidal epithelial cells with regular nuclei in through a chondromyxoid-like stroma.
Because the tumor was located in the buccal mucosa, the treatment of choice was excision. This approach with assessment of surgical margins seems to be the most appropriate initial therapy, since the treatment is effective and has an excellent prognosis when surgery is performed properly with a cure rate of 95% of cases [19].
Pleomorphic adenoma, despite being a benign tumor and characterized microscopically as an encapsulated tumor, has microscopic pseudopods with extension to the surrounding tissue, to which the pseudocapsule yields [18]. The rupture of the tumor capsule can considerably increase the chances of recurrence, highlighting the importance of an adequate dissection technique [20]. The integrity of the tumor capsule was maintained in this case, thereby minimizing the rate of recurrence of the neoplasia.
The patient in question has been followed-up for approximately one year and has not shown any evidence of recurrence. Follow-up after excision of the lesion must be performed for a minimum of five years [21].
Conclusion
The occurrence of pleomorphic adenoma in the buccal mucosa is uncommon. The complete excision of the lesion under local anesthesia allowed the patient to heal and prevented a possible malignant transformation, with little associated morbidity.
REFERENCES
1.
2.
3.
Gomes JPP, Veloso JRC, Altemani AMAM, et al. Three-dimensional volume imaging to increase the accuracy of surgical management in a case of recurrent chordoma of the clivus. Am J Case Rep 2018;19:1168–74. [CrossRef]
[Pubmed]

4.
Erdem MA, Cankaya AB, Güven G, Olgaç V, Kasapoğlu C. Pleomorphic adenoma of the palate. J Craniofac Surg 2011;22(3):1131–4. [CrossRef]
[Pubmed]

5.
Clauser L, Mandrioli S, Dallera V, Sarti E, Galiè M, Cavazzini L. Pleomorphic adenoma of the palate. J Craniofac Surg 2004;15(6):1026–9. [CrossRef]
[Pubmed]

6.
Haltiner CC, Betz S, Smith J, Nelson B, Ambrosio AA. Carcinoma ex-pleomorphic adenoma diagnosis during global health engagement operations. Mil Med 2021;186(Suppl 1):828–32. [CrossRef]
[Pubmed]

7.
Debnath SC, Saikia AK, Debnath A. Pleomorphic adenoma of the palate. J Maxillofac Oral Surg 2010;9(4):420–3. [CrossRef]
[Pubmed]

8.
Nourwali I, Dar-Odeh N. Pleomorphic adenoma in the lower lip: A case report and a review. Eur J Dent 2019;13(4):649–53. [CrossRef]
[Pubmed]

9.
10.
Periasamy S, Manoharan A, Garg H, Kumar SP. Pleomorphic adenoma of the cheek: A case report. 2019;11(8):e5312. [CrossRef]
[Pubmed]

11.
Seok J, Hyun SJ, Jeong WJ, Ahn SH, Kim H, Jung YH. The difference in the clinical features between carcinoma ex pleomorphic adenoma and pleomorphic adenoma. Ear Nose Throat J 2019;98(8):504–9. [CrossRef]
[Pubmed]

12.
Cohen MA. Pleomorphic adenoma of the cheek. Int J Oral Maxillofac Surg 1986;15(6):777–9. [CrossRef]
[Pubmed]

13.
Babu SS, Sunil S, Prathap A, Mathew AL. Acinic cell carcinoma of the posterior buccal mucosa: A rare case report. J Cancer Res Ther 2020;16(3):675–9. [CrossRef]
[Pubmed]

14.
Tiago RSL, Castro GA, Ricardo LAC, Biihler RB, Fava AS. Adenoma pleomórfico de parótida: Aspectosclínicos, diagnósticos e terapêuticos. Rev Bras Otorrinolaringol 2003;69(4):485–9. [CrossRef]

15.
Stodulski D, Rzepko R, Kowalska B, Stankiewicz C. Carcinoma ex pleomorphic adenoma of major salivary glands—a clinicopathologic review. Otolaryngol Pol 2007;61(5):687–93. [CrossRef]
[Pubmed]

16.
Passi D, Ram H, Dutta SR, Revansidha Malkunje L. Pleomorphic adenoma of soft palate: Unusual occurrence of the major tumor in minor salivary gland – A case report and literature review. J Maxillofac Oral Surg 2017;16(4):500–5. [CrossRef]
[Pubmed]

17.
van der Wal JE, Leverstein H, Snow GB, Kraaijenhagen HA, van der Waal I. Parotid gland tumors: Histologic reevaluation and reclassification of 478 cases. Head Neck 1998;20(3):204–7.
[Pubmed]

18.
Varghese BT, Sebastian P, Abraham EK, Mathews A. Pleomorphic adenoma of minor salivary gland in the parapharyngeal space. World J Surg Oncol 2003;1(1):2. [CrossRef]
[Pubmed]

19.
Dhir P, David CM, Dhaduti K G. Pleomorphic adenoma of the parotid gland with cystic degeneration: A rare case report. J Indian Acad Oral Med Radiol 2015;26(4):450–3. [CrossRef]

20.
Dhanutai K, Sappayatosok K, Kongin K. Pleomorphic adenoma of the palate in a child: A case report. Med Oral Patol Oral Cir Bucal Bangkok 2009;14(2):73–5.
[Pubmed]

21.
Pérez-de-Oliveira, ME, Leonel AC, de Castro JF, Carvalho EJ, Vargas PA, Perez DE. Histopathological findings of intraoral pleomorphic adenomas: A retrospective study of a case series. Int J Surg Pathol 2019;27(7):729–35. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Rhaina Anuá Souza Afonso - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Géssica Vasconcelos Godinho - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Bianca Barchetta de Nápoles Albuquerque - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Luiz Evaristo Ricci Volpato - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Rhaina Anuá Souza Afonso et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.