|
Case Report
Abdominal tuberculosis masquerading as carcinomatosis: Not difficult to miss!
1 Acute Clinical Fellow, General Surgery, Royal Derby Hospital, Derby, United Kingdom
2 Registrar, General Surgery, Royal Derby Hospital, Derby, United Kingdom
3 Consultant, Vascular Surgery, Royal Derby Hospital, Derby, United Kingdom
Address correspondence to:
Christiana O Fabelurin
No. 46 Auriga Court, Little Chester, Derby, DE1 3RH,
United Kingdom
Message to Corresponding Author
Article ID: 101208Z01CF2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Fabelurin CO, Arora D, Abayasekara K. Abdominal tuberculosis masquerading as carcinomatosis: Not difficult to miss! Int J Case Rep Images 2021;12:101208Z01CF2021.ABSTRACT
Introduction: Abdominal tuberculosis (ATB) is a rare extrapulmonary manifestation of Mycobacterium tuberculosis infection. It usually presents with non-specific symptoms that can mimic other intra-abdominal conditions like acute appendicitis, Crohn’s disease, ovarian pathology, and intra-peritoneal carcinomatosis and is therefore, easy to overlook. Diagnosing ATB in the pediatrics population tends to be even more challenging as an obvious history of exposure may be difficult to obtain. Chronicity of symptoms and lack of Bacillus Calmette-Guérin (BCG) scar should raise suspicion. Diagnostic laparoscopic biopsy and histopathology provides definitive diagnosis.
Case Report: This case report presents the case of a 16-year-old girl with a history of recurrent abdominal pain, vomiting, and pyrexia. At initial diagnostic laparoscopy, she underwent laparoscopic appendectomy. Vesicles were noted in the pelvis. The patient failed to improve. Exposure to tuberculosis (TB) was denied. Review of pre-operative computed tomography (CT), comprehensive re-laparoscopy, and histopathology of appendix were used for final diagnosis of this condition. The patient was treated using anti-TB therapy for six months following which, she was able to make a full recovery.
Conclusion: Abdominal TB is very difficult to diagnose in young patients and should be considered in those presenting with vague, recurrent, or persistent abdominal symptoms. A high index of suspicion is needed for early diagnosis and prompt treatment of this condition. In patients with low or no identifiable risk factors for TB, definitive diagnosis is justified prior to the initiation of therapy.
Keywords: Abdominal cavity, Pediatrics, Peritonitis, Tuberculosis
Introduction
Tuberculosis (TB) is a contagious disease that is a major cause of illness and remains one of the most common causes of death worldwide [1]. In the United Kingdom (UK), the incidence of TB in 2019 fell to the lowest recorded level since 1960; however, it remains rampant worldwide [1],[2],[3].
Ranking above Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome (HIV/AIDS), TB remains the leading cause of death from a single infectious agent [1].
Tuberculosis is caused by Mycobacterium tuberculosis and typically affects the lungs but can also affect other sites [1],[4]. Abdominal tuberculosis (ATB) accounts for 5% cases of extrapulmonary TB and refers to infection of the gastrointestinal tract (GIT), the mesentery, and its nodes, omentum, peritoneum, and related solid organs [3],[5],[6]. It usually presents in a clinical spectrum that ranges from non-specific symptoms to those that mimic Crohn’s disease or abdominal carcinomatosis [5],[7],[8],[9]. Peritoneal TB (PTB) is a very rare form of TB and accounts for only 1–2% of cases of TB, 31–58% of cases of abdominal TB [9].
Abdominal TB tends to present as a subacute disease and most common clinical manifestations include ascites, abdominal pain, fever, abdominal distension, constipation/diarrhea, hepatomegaly, splenomegaly, weight loss, anorexia, and malaise [9]. Risk factors for extrapulmonary TB include HIV, cirrhosis, diabetes mellitus, female gender, extremes of age, Asian/African ethnicity, malignancy, and peritoneal dialysis treatment [3],[7],[9],[10]. The incidence of ATB tends to be higher among school children and adolescents than in children under 5 years old [6],[11].
The multi-faceted presentation of ATB makes its diagnosis a challenge in healthcare, particularly in the pediatrics population, where the clinical presentations may differ from those of adults. In most cases, children’s inability to characterize their problems accurately may lead to delays in diagnosis and treatment initiation [12].
In this case report, we present a case of a 16-year-old girl who had no risk factors for ATB, no concomitant pulmonary TB or tuberculous contact but developed abdominal TB which shows that although rare, ATB can also occur in the pediatrics population.
Case Report
A 16-year-old girl presented to the hospital with complaints of on-going central and right-sided lower abdominal pain. She had visited Slovakia the month before and attended a hospital in Slovakia with these complaints. She had an abdominal ultrasound which showed free fluid in the pelvis for which she was treated on intravenous antibiotics.
On presentation to our hospital, she had abdominal pain and nausea but denied any urinary symptoms/vomiting/fever. On examination, she appeared to be systemically well, her abdomen was soft with central and right iliac fossa tenderness. Rovsing’s sign was positive. Her urinalysis was negative. Bloods including inflammatory markers were all within normal range. Her pelvic ultrasound showed a 6.0 × 5.4 × 3.4 cm simple cyst within the right adnexal region, superior, adjacent, and separate to this were two smaller simple cysts measuring 10 mm and 7 mm in diameter. Her left ovary was normal.
The working diagnosis by gynecology department was right ovarian cyst and she was discharged with a plan for clinic follow-up with tumor markers and a repeat pelvic ultrasound. Cancer antigen 125 (CA-125) level was 301 (Normal range is 0–35 kU/L), but the other tumor markers were normal.
She re-presented to the emergency department a few times with similar symptoms. On one of the presentations, she described her pain as constant “pins and needles” sensation. She had a low-grade pyrexia. Her blood showed normal renal function and raised inflammatory markers. Computed tomography (CT) abdomen pelvis showed a right ovarian cyst but could not exclude an ovarian torsion. She was taken to theatre for a diagnostic laparoscopy where an inflamed appendix was identified and removed.
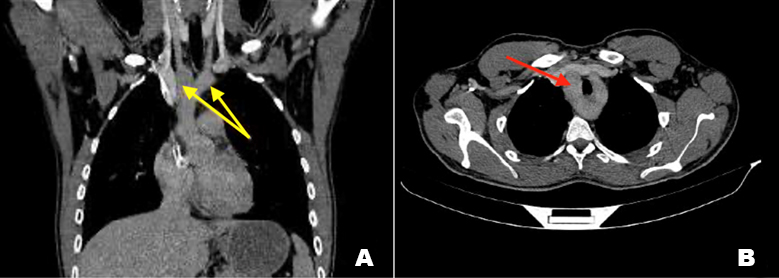
She continued to be unwell post-operatively (post-op) and her inflammatory markers were worsening, so an abdominal ultrasound was requested to rule out a post-op collection. However, this could not be carried out as she was extremely tender during the procedure. Her previous CT scan was reviewed, and a new post-operative CT abdomen and pelvis was performed, both of which revealed an extensive peritoneal thickening and enhancement, some of which was extremely nodular and quite concerning (Figure 1). The radiologist advised that the nodularity seen is unusual in peritonitis and laparoscopic biopsy should be considered for diagnostic purposes. There was no deep collection noted on CT.
Diagnostic laparoscopy and omental biopsy were performed during the same hospital admission. Intraoperative findings included an omental cake with small volume nodules on the small bowel serosa and ascites.
Omental biopsy histology showed a granulomatous inflammation with special staining suggesting mycobacterial infection (Figure 2 and Figure 3). Ascitic fluid also showed histiocytic aggregates, which were highly suspicious of tuberculous peritonitis. There were no malignant cells seen. She had a chest X-ray and an echocardiogram (ECHO) which were both normal and showed no evidence of pulmonary and pericardial TB. Antinuclear antibody (ANA) screen was positive, but all other immunological tests were normal. She was commenced on TB treatment for ATB, following which she was able to achieve a full recovery after a six-month anti-TB therapy.
Discussion
Tuberculosis in children tends to be more common in TB-endemic countries. Over the last 20 years, the UK has seen a general decline in the incidence of pulmonary TB, but a rise in extrapulmonary TB, especially among non-UK born patients [2],[10],[13],[14]. Worldwide, the risk of abdominal TB in children increases with deterioration in socioeconomic status and increased frequency of HIV infection [8],[10],[13],[15]. As a result, HIV testing is recommended to all patients presenting with TB [1]. Tuberculous peritonitis is a very rare form of TB with an incidence of 1–2% of all cases of TB and is primarily seen in adults [9],[16]. In England, ATB is rare and requires a high index of suspicion in areas with a large immigrant population and in areas which are overcrowded and nutritionally deficient [2].
Abdominal TB poses even more of a diagnostic challenge in the pediatrics population due to the varied presentation ranging from non-specific symptoms to those that mimic common abdominal conditions [6]. The most common presentations in children include fever, abdominal pain±discomfort, weight loss, and ascites [1],[3],[7],[12],[17],[18]. This is evident in this case study as the patient had presented to the hospital several times and had been diagnosed with other common intra-abdominal conditions (appendicitis and ovarian cysts) before ATB was diagnosed. The initial diagnosis of acute appendicitis when reviewed in context was changed to granulomatous appendicitis in keeping with TB appendicitis in this patient.
Tuberculosis infects the abdomen and peritoneum through several mechanisms such as ingestion of contaminated products, hematogenous spread, direct spread, and by lymphatic spread from a primary source [3],[6],[7],[9],[17],[18]
There are several clinical and laboratory tests that can be employed in the diagnosis of TB. These include tuberculin skin test, interferon gamma release assay, hematologic studies, peritoneal fluid analysis, laparoscopic biopsies, mycobacterial culture, and nucleic acid amplification test [3],[7],[9],[17],[19]. The type of investigation employed depends on the site of involvement. For ATB, laparoscopy with target peritoneal biopsy is the current investigation of choice for diagnosis [3],[19]. In our patient, a diagnostic laparoscopy for evaluation and culture of ascitic fluid and omental biopsies were used to confirm diagnosis.
Imaging studies are also immensely helpful in diagnosing ATB [3]. In children, ultrasound can be used as a first line imaging to avoid exposure to radiation. In addition, it is simple, reliable, non-invasive, and easily accessible [7],[17]. Possible ultrasound findings may include ascites and mesenteric lymphadenopathy [4],[11]. In peritoneal disease, ascitic fluid with strands, fine septae, and debris are typically seen on ultrasound [4],[9],[17]. Computed tomography is also useful in the diagnosis of ATB by imaging. The visualization of a smooth peritoneum with minimal thickening and pronounced enhancement, as well as omental thickening and nodularity on CT are indicative of PTB [4],[9],[18]. Imaging studies may also act as a guide in helping to decide where and how biopsies should be obtained [4].
A chest X-ray performed on our patient was negative for pulmonary TB; however, it is vital that all patients who present with extrapulmonary TB undergo investigations to rule out pulmonary TB as a primary source. Several studies have shown that more than half of patients who present with extrapulmonary TB will have concomitant pulmonary TB [1],[11],[18],[20].
Abdominal TB in children is rare and has negative emotional and psychological effects, which is why TB therapy should be tailored to treat the patient holistically. Tuberculosis eradication therapy is to be commenced as soon as TB is diagnosed. Some studies suggest starting empirical treatment of TB when there is a high index of suspicion [3],[4],[5],[9]. The length of treatment of extrapulmonary TB in children is unclear; however, most studies have shown that there is no difference in result in patients where a prolonged therapy (more than six months) was adopted [7],[16],[19],[21]. The classic 4-drug anti-TB medications (Rifampicin, Ethambutol, Isoniazid, and Pyrazinamide) were used for the patient in this case study, over a period of six months and a favorable outcome was achieved.
Conclusion
Abdominal TB is difficult to diagnose in young patients and should be considered in those presenting with vague, recurrent, or persistent abdominal symptoms, especially in areas of low endemicity. The chronicity of clinical features in our patient should have raised an early suspicion of ATB. In patients with low or no identifiable risk factors for TB, definitive diagnosis is justified prior to the initiation of therapy.
REFERENCES
1.
Guidance for National Tuberculosis Programmes on the Management of Tuberculosis in Children. 2ed. Switzerland: World Health Organisation; 2014. [Available at: https://apps.who.int/iris/bitstream/handle/10665/112360/9789241548748_eng.pdf;jses sionid=569F41DEB41BF5D950CB29864FC0E7FF?sequence=1]

2.
Public Health England. Tuberculosis in England 2019 report. [https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943356/TB_Annual_Report_2020.pdf]

3.
Sanai FM, Bzeizi KI. Systematic review: Tuberculous peritonitis – presenting features, diagnostic strategies, and treatment. Aliment Pharmacol Ther 2005;22(8):685–700. [CrossRef]
[Pubmed]

4.
Zaslavsky J, Mulugeta-Gordon L, Vasko I, et al. Tuberculous peritonitis in children: Two case reports highlighting the important role of imaging. Radiol Case Rep 2018;13(4):862–6. [CrossRef]
[Pubmed]

5.
Malik R, Srivastava A, Yachha SK, Poddar U, Lal R. Childhood abdominal tuberculosis: Disease patterns, diagnosis, and drug resistance. Indian J Gastroenterol 2015;34(6);418–25. [CrossRef]
[Pubmed]

6.
Shrestha D. Shrestha MK, Raya GB, et al. A 14-year-old girl presenting with tuberculous intestinal perforation while in a temporary shelter after the 2015 earthquake in Nepal. Paediatr Int Child Health 2018;38(1):69–72. [CrossRef]
[Pubmed]

7.
Avcu G, Sensoy G, Karli A, et al. A case of tuberculous peritonitis in childhood. J Infect Public Health 2015;8(4):369–72. [CrossRef]
[Pubmed]

8.
Mirza B, Ijaz L, Saleem M, Sheikh A. Surgical aspects of intestinal tuberculosis in children: Our experience. Afr J Paediatr Surg 2011;8(2):185–9. [CrossRef]
[Pubmed]

9.
National Library of Medicine, or "Vancouver style" (International Committee of Medical Journal Editors): DynaMed. Ipswich (MA): EBSCO Information Services. 1995. Record No. T910286, Abdominal Tuberculosis. [Available at: https://www.dynamed.com/condition/abdominal-tuberculosis]

10.
Hayward S, Harding RM, McShane H, Tanner R. Factors influencing the higher incidence of tuberculosis among migrants and ethnic minorities in the UK. F1000Res 2018;7:461. [CrossRef]
[Pubmed]

11.
K?l?ç Ö, Somer A, Törün SH, et al. Assessment of 35 children with abdominal tuberculosis. Turk J Gastroenterol 2015;26(2):128–32. [CrossRef]
[Pubmed]

12.
Basu S, Ganguly S, Chandra PK, Basu S. Clinical profile and outcome of abdominal tuberculosis in Indian children. Singapore Med J 2007;48(10):900–5.
[Pubmed]

14.
Kruijshaar ME, Abubakar I. Increase in extrapulmonary tuberculosis in England and Wales 1999–2006. Thorax 2009;64(12):1090–5. [CrossRef]
[Pubmed]

15.
Lambrianides AL, Ackroyd N, Shorey BA. Abdominal tuberculosis. Br J Surg 1980;67(12):887–9. [CrossRef]
[Pubmed]

16.
Jullien S, Jain S, Ryan H, Ahuja V. Six-month therapy for abdominal tuberculosis. Cochrane Database Syst Rev 2016;11(11):CD012163. [CrossRef]
[Pubmed]

17.
Tinsa F, Essaddam L, Fitouri Z, et al. Abdominal tuberculosis in children. J Pediatr Gastroenterol Nutr 2010;50(6):634–8.
[Pubmed]

18.
Lin YS, Huang YC, Lin TY. Abdominal tuberculosis in children: A diagnostic challenge. J Microbiol Immunol Infect 2010;43(3);188–93. [CrossRef]
[Pubmed]

19.
Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul) 2015;78(2):47–55. [CrossRef]
[Pubmed]

20.
Cruz AT, Starke JR. Clinical manifestations of tuberculosis in children. Paediatr Respir Rev 2007;8(2):107–17. [CrossRef]
[Pubmed]

21.
Nahid P, Dorman SE, Alipanah N, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis 2016;63(7):e147–95. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Christiana O Fabelurin - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Deeksha Arora - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Kumar Abayasekara - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementThere was no written consent obtained from this patient as there were no patient identifying factors used in the article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Christiana O Fabelurin et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.