|
Case Report
Bilateral nephroblastoma: A case report
1 Department of Pediatric Imaging, Pediatric Teaching Hospital, Rabat, Morocco
Address correspondence to:
Kaoutar Imrani
Rabat Children’s Hospital, Mohamed V University, Rabat,
Morocco
Message to Corresponding Author
Article ID: 101158Z01KI2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Imrani K, Amalik S, Allali N, El Haddad S, Chat L. Bilateral nephroblastoma: A case report. Int J Case Rep Images 2020;11:101158Z01KI2020.ABSTRACT
Bilateral nephroblastoma represents 4–8% of all Wilms′ tumors (WTs). Nephroblastomatosis (NB) is defined by the presence of multiple or diffuse nephrogenic rests (NRs). These lesions are always present in bilateral nephroblastoma, and they are better detected by computed tomography (CT). Treatment consists of a homogeneous therapeutic approach combining chemotherapy, surgery, and radiotherapy. The rarity of bilateral nephroblastoma associated with NB explains the variability of the therapeutic proposals and the lack of codified protocols. We report the case of an 18-month-old boy presenting bilateral nephroblastoma with NB.
Keywords: Bilateral nephroblastoma, Children, Nephroblastomatosis
Introduction
Nephroblastoma is an embryonic tumor occurring in early childhood. It is exceptional in adults. Almost 95% of kidney tumors in children are nephroblastomas. Bilateral localization, either immediately or secondarily is rare, it represents 4–8% of all WTs. This shape occurs in younger children, often associated with NB [1],[2],[3].
Nephroblastomatosis is defined by the presence of NRs. In unilateral WTs, NRs are usually only detectable by histology whereas in bilateral WT, they can be seen on imaging. Abdominal ultrasound and chest X-rays are used as a first line diagnosis tool. A CT, or a magnetic resonance imaging (MRI), is performed in a second time to confirm the ultrasound data [2],[4],[5].
We report the case of an 18-month-old boy admitted for bilateral nephroblastoma with NB.
The aim of this article is to demonstrate the challenge of imaging findings that lead to the diagnosis and to show therapeutic modalities.
Case Report
An 18-month-old boy was admitted for an abdominal mass. The clinical examination found a mass in the right hypochondrium extending to the right flank. Biologically the patient had elevated lactate dehydrogenase (LDH) (580 U/L) and CRP (16 mg/dL).
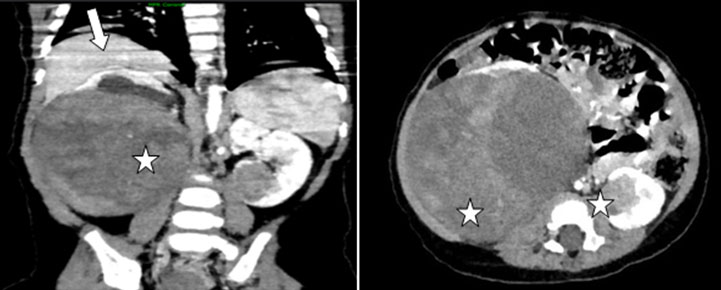
The abdominal ultrasound showed a hyperechoic and heterogeneous bilateral renal mass and demonstrated hypoechoic cortical nodularity related to NB lesions (Figure 1). The abdominal CT scan after intravenous contrast agent injection showed bilateral renal masses measuring 11 cm on the right and 3 cm on the left, hypodense evoking a bilateral nephroblastoma (Figure 2). There was no invasion of the renal vein and the inferior vena cava. However, NB lesions could not be detected.
Staging CT of the thorax, abdomen, and pelvis (CT-TAP) showed no distant metastasis.
After multidisciplinary concentration meeting (RCM) the infant received preoperative chemotherapy based on vincristine (1.5 mg/m2) and actinomycin D (15 μg/kg) for four weeks, which allowed tumor regression from 11 cm on the right to 6 cm and from 3 cm on the left to 1.5 cm.
The patient was operated at the age of 24 months. Surgical exploration found bilateral nephroblastoma with NB. The right-sided tumor was removed by subtotal nephrectomy. The left lower pole tumor was resected with an ultrasonic knife. Histological report was bilateral NB with a multicentric WT of favorable histology. The operation was followed by further chemotherapy with vincristine and actinomycin for 12 weeks. The patient was followed up every 3–6 months and an abdominal ultrasound was performed every 6 months. After 62 months of diagnosis, there has been no evidence of recurrence or tumor progression on abdominal ultrasound and the patient is in a good clinical condition.
Discussion
Kidney tumors account for 5–8% of childhood cancers, they are more common in children under 6 years of age. Almost 95% of these tumors are nephroblastomas. Bilateral nephroblastoma represents 4–8% of cases [2],[3].
Nephroblastomatosis is defined by the presence of multiple or diffuse NRs. They are observed in 12–17% of operative piece of nephrectomy in unilateral nephroblastoma and up to 100% of cases in bilateral nephroblastoma. This association suggests that NRs are associated with the same physiopathogenic phenomenon and could be a precursor lesion of nephroblastoma [3],[4].
Two categories of NR are recognized: intralobar (ILNR) and perilobar (PLNR). Perilobar nephrogenic rest is found in 1% of pediatric autopsies, while intralobar form is found only in 0.1%. In unilateral WT, NRs are usually only detectable by histology whereas in bilateral WT, they can be seen on imaging [1],[2],[5].
The presence of NRs within a nephrectomy for nephroblastoma exposes the patient to the risk of contralateral tumor. This risk is even greater for children under one year of age [4],[6]. The diagnosis of nephroblastoma can be suspected clinically and radiologically but requires histological confirmation [5].
Clinically, nephroblastoma can be revealed by abdominal pain or a palpable abdominal mass. More rarely, the patient can present with hematuria, fever, or high blood pressure [6],[7],[8].
Abdominal ultrasound and chest X-rays are used as a first line diagnosis tool. A CT, or an MRI, is performed in a second time to confirm the ultrasound data. An abdominal and pelvic CT scan is realized before and after contrast injection on portal phase. The chest CT is performed during the injection acquisition if there are suspicious lesions on chest X-ray [7],[8].
The role of imaging is to combine the arguments of the diagnosis of nephroblastoma and to look for associated abnormalities (“horseshoe” kidney or other urogenital malformations can change the therapeutic attitude) [6],[7],[8].
Imaging findings of nephroblastoma depend on the different components of the tumor (necrosis, hemorrhage, calcification, and fat). The characteristic signs are the presence of a solid mass well defined with pseudocapsule, realizing a rind or “claw” of renal parenchyma surrounding the tumor [6].
Ultrasound (US) is often the first line investigation in pediatrics, particularly for those presenting with an abdominal mass. Nephroblastomas appear as solid, heterogeneous masses with calcification, but are rarely cystic on US.
Nephroblastomatosis lesions are presented in US as images often hypoechoic but can also be hyperechoic, isoechoic, anechoic, nodular, or diffuse. Computed tomography performs better than US by showing nodular or diffuse, isodense lesions that do not enhance after contrast injection. On MRI, NB lesions are iso-intense that become hypo-intense in T1 after gadolinium injection [3],[4],[5].
The classic histological aspect is that of a three-phase nephroblastoma, associating with blastema, epithelial differentiation, and stromal differentiation in variable proportions [1],[7].
Treatment consists of a homogeneous therapeutic approach combining with chemotherapy, surgery, and radiotherapy. The rarity of bilateral nephroblastoma associated with NB explains the variability of the therapeutic proposals and the lack of codified protocols. Management must be multidisciplinary and must respond to two contradictory imperatives: to be as curative as possible and to preserve the maximum renal parenchyma to avoid progression to renal failure. Bilateral nephroblastoma is treated with preoperative chemotherapy followed by surgery then postoperative chemotherapy, sometimes associated with radiotherapy [7],[8].
Conclusion
Nephroblastomatosis lesions are always present in bilateral nephroblastoma. The CT scan is more performant in the detection of these lesions; however, it can be detected by an abdominal ultrasound (as in our case). The management of bilateral NB is binding and the therapeutic decision must be made after multidisciplinary consultation meeting.
REFERENCES
1.
Charlton J, Irtan S, Bergeron C, Pritchard-Jones K. Bilateral Wilms tumour: A review of clinical and molecular features. Expert Rev Mol Med 2017;19:e8. [CrossRef]
[Pubmed]

2.
Perlman E, Boccon-Gibod L. Kidney tumors in childhood. [Article in French]. Ann Pathol 2004;24(6):516–35. [CrossRef]
[Pubmed]

3.
Jouini R, Maazoun K, Chelly S, Mekki M, Belgnith M, Nouri A. Nephroblastoma and Wilms tumor: Report of 2 cases. [Article in French]. Prog Urol 2003;13(2):273–6.
[Pubmed]

4.
Shamberger RC, Haase GM, Argani P, et al. Bilateral Wilms’ tumors with progressive or nonresponsive disease. J Pediatr Surg 2006;41(4):652–7. [CrossRef]
[Pubmed]

5.
Telander RL, Gilchrist GS, Burgert EO Jr, Kelalis PP, Goellner JR. Bilateral massive nephroblastomatosis in infancy. J Pediatr Surg 1978;13(2):163–6. [CrossRef]
[Pubmed]

6.
Sethi AT, Narla LD, Fitch SJ, Frable WJ. Best cases from the AFIP: Wilms tumor in the setting of bilateral nephroblastomatosis. Radiographics 2010;30(5):1421–5. [CrossRef]
[Pubmed]

7.
Dumba M, Jawad N, Mchugh K. Neuroblastoma and nephroblastoma: A radiological review. Cancer Imaging 2015;15(1):5. [CrossRef]
[Pubmed]

8.
Paya K, Horcher E, Lawrenz K, Rebhandl W, Zoubek A. Bilateral Wilms’ tumor - surgical aspects. Eur J Pediatr Surg 2001;11(2):99–104. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Kaoutar Imrani - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sanae Amalik - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nazik Allali - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Siham El Haddad - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Latifa Chat - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Kaoutar Imrani et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.