|
Case Report
Intramural gestation: A rare localization of ectopic pregnancy
1 Radiology Department, Maternity and Children’s Hospital of Rabat, Morocco
2 Sarah Moumna, Radiology Department, Maternity and Children’s Hospital of Rabat, Morocco
Address correspondence to:
Sarah Moumna
Radiology Department, Maternity and Children’s Hospital of Rabat,
Morocco
Message to Corresponding Author
Article ID: 101087Z01SM2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Moumna S, El Ghorfi S, El Haddad S, Allali N, Chat L. Intramural gestation: A rare localization of ectopic pregnancy. Int J Case Rep Images 2020;11:101087Z01SM2020.ABSTRACT
Introduction: Intramural pregnancy is a rare form of ectopic pregnancy; it is defined by a gestation within the uterine wall, completely surrounded by myometrium and separated from the uterine cavity and the fallopian tube. Preoperative diagnosis is difficult and hysterectomy may be required due to delay in diagnosis.
Case Report: We report a rare case of intramural ectopic pregnancy diagnosed by sonography and treated surgically.
Conclusion: Early detection of intramural ectopic pregnancy is needed to prevent complications like uterine rupture and helps preserve fertility.
Keywords: Ectopic pregnancy, Intramural, Ultrasonography
Introduction
Intramural pregnancy, defined as gestation completely surrounded by the myometrium located within the uterine wall with separation from the uterine cavity, fallopian tube, or round ligament, is an extremely rare form of pregnancy and less than 50 cases have been reported in literature (less than 1% of all ectopic pregnancy) [1]. In most cases, fetal wastage occurs at 11–22 weeks’ gestation due to maternal hemoperitoneum and hypovolemic shock [2].
Careful ultrasound examination can help establish the diagnosis [3]. It usually shows an ectopic gestational sac with a yolk sac that is distinct from the endometrium cavity, yet within the uterus [4].
Intramural ectopic pregnancies are at risk of rupture and may require surgical intervention. Hysterectomy is most often unavoidable, because of extensive bleeding. However, early management of patients with unruptured ectopic pregnancies would give these patients the chance to preserve their fertility.
Case Report
We report a rare case of intramyometrial ectopic pregnancy in a 36-year-old woman, gravida 2, para 2 (her first pregnancy was a first trimester complete spontaneous miscarriage), who presented to the emergency department with complaints of lower abdominal pain. There was no history of vaginal bleeding.
Her last menstrual period was nine weeks before. Physical examination revealed stable vital signs while bimanual examination revealed an enlarged uterus with no adnexal masses. The serum beta-human chorionic gonadotropin level was 79,000 mIU/mL at the time of diagnosis.
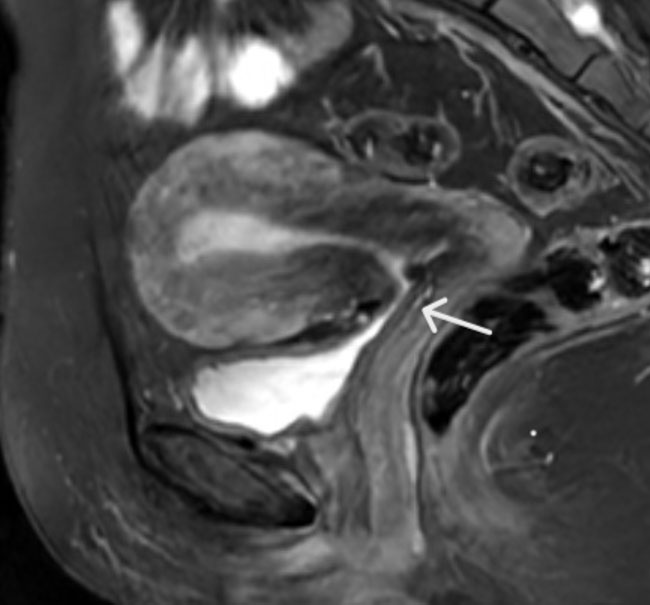
Abdominal ultrasound revealed a gestational sac with a heartbeating fetus along measuring 19.6 mm corresponding to nine weeks gestation (Figure 1). The endometrial cavity was empty and both the endometrium and gestational sac appeared to be surrounded by myometrium (Figure 2). There was no blood in the pouch of Douglas. A diagnosis of an intramural ectopic pregnancy was made and the patient taken to operating room.
At laparoscopy a 3.8 × 2 cm ectopic pregnancy was found to have ruptured through the posterior wall of the uterus. The site of rupture was posterior, inferior, and medial to the origin of the right Fallopian tube. Both Fallopian tubes appeared normal throughout their entire length. There was 300 mL of hemoperitoneum and active bleeding from the site of the ectopic pregnancy. That is why we did need to perform a hysterectomy. She had a satisfactory recovery.
Histological examination confirmed chorionic villi surrounded by myometrium with no identifiable Fallopian tube, confirming a diagnosis of intramural ectopic pregnancy.
Discussion
Ectopic pregnancy is the most common gynecologic abnormality and emergency that afflicts a potential mother and remains a major cause of mortality worldwide.
Intramural ectopic pregnancy is one of the rare forms of ectopic pregnancy, and the world literature had only a handful of cases reported to date [5],[6]. It refers to a uterine conception in which implantation occurs in the myometrium, separated from the endometrial cavity, fallopian tubes, or round ligament [4]. Twelve weeks of gestation are rarely exceeded in intramyometrial gestation with risk of uterine rupture and 2.5% of maternal mortality [7].
Several etiologies have been proposed to explain the existence of this rare condition. The most common factor is uterine trauma, such as previous curettage, cesarean section, and myomectomy [8],[9]. Intramural pregnancy may also occur within foci of adenomyosis [4]. Another scenario is that the embryo may be implanted inside the myometrium artificially during embryo transfer in in vitro fertilization [10]. In our case no risk factors were identified.
Abdominal pain and uterine bleeding in the presence of a positive pregnancy test are the hallmark signs of an ectopic pregnancy. Early diagnosis may not be easy by ultrasound and mostly made intraoperatively.
The typical ultrasound appearance of intramural pregnancy is a gestational sac completely surrounded by myometrium [11] as described in our case. The uterine cavity is empty and no adnexal lesions are visualized.
Magnetic resonance imaging (MRI) confirms the location of the gestational sac and demonstrates no communication with the endometrial cavity and provides better visualization of the myometrium and endometrium separately. In our case, MRI was not performed due to the increasing pain and the maternal prognosis.
The treatment for patients with intramural pregnancy should be individualized, depending on the location of the lesion, depth of muscular invasion, gestational age, and the desire for future fertility [1].
Prognosis is very poor for fetuses in intramural pregnancies. The treatment remains surgery. With uterine rupture and hypovolemic shock, emergency hysterectomy is often necessary. With better methods of earlier detection and preoperative diagnosis of unruptured intramural ectopic pregnancy, conservative or expectant management could be offered to preserve the patient’s fertility.
Conclusion
Intramural pregnancy is the rarest form of ectopic pregnancy and is a life-threatening condition. Early detection of intramural pregnancy is needed to prevent complications, such as uterine rupture, and early management of these patients would give them the chance to preserve their fertility. It is possible to diagnose them preoperatively on ultrasound but even the most experienced sonographers may only see a handful during their lifetime.
REFERENCES
1.
Boukhanni L, Ait Benkaddour Y, Bassir A, Aboulfalah A, Asmouki H, Soummani A. A rare localization of ectopic pregnancy: Intramyometrial pregnancy in twin pregnancy following IVF. Case Rep Obstet Gynecol 2014;2014:893935. [CrossRef]
[Pubmed]

2.
Fait G, Goyert G, Sundareson A, Pickens A Jr. Intramural pregnancy with fetal survival: Case history and discussion of etiologic factors. Obstet Gynecol 1987;70(3 Pt 2):472–4.
[Pubmed]

3.
Bernstein HB, Thrall MM, Clark WB. Expectant management of intramural ectopic pregnancy. Obstet Gynecol 2001;97(5 Pt 2):826–7. [CrossRef]
[Pubmed]

4.
Ginsburg KA, Quereshi F, Thomas M, Snowman B. Intramural ectopic pregnancy implanting in adenomyosis. Fertil Steril 1989;51(2):354–6. [CrossRef]
[Pubmed]

5.
Ong C, Su LL, Chia D, Choolani M, Biswas A. Sonographic diagnosis and successful medical management of an intramural ectopic pregnancy. J Clin Ultrasound 2010;38(6):320–4. [CrossRef]
[Pubmed]

6.
Ko HS, Lee Y, Lee HJ, et al. Sonographic and MRI findings in 2 cases of intramural pregnancy. J Clin Ultrasound 2006;34(7):356–60. [CrossRef]
[Pubmed]

7.
Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update 2014;20(2):250–61. [CrossRef]
[Pubmed]

8.
Lee GS, Hur SY, Kown I, Shin JC, Kim SP, Kim SJ. Diagnosis of early intramural ectopic pregnancy. J Clin Ultrasound 2005;33(4):190–2. [CrossRef]
[Pubmed]

9.
Ko HS, Lee Y, Lee HJ, et al. Sonographic and MR findings in 2 cases of intramural pregnancy treated conservatively. J Clin Ultrasound 2006;34(7):356–60. [CrossRef]
[Pubmed]

10.
Khalifa Y, Redgment CJ, Yazdani N, Taranissi M, Craft IL. Intramural pregnancy following difficult embryo transfer. Hum Reprod 1994;9(12):2427–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Sarah Moumna - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Salma El Ghorfi - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Siham El Haddad - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nazik Allali - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Latifa Chat - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Sarah Moumna et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.